Testosterone therapy isn’t “safe” or “dangerous” in the abstract—only in the context of a verified diagnosis.
The Hormone–Prostate Link (Myths vs Facts)
On one side: “TRT causes prostate cancer.”
On the other: “TRT is harmless—if you want it, take it.”
And caught in the middle is a man who simply wants to sleep through the night, feel like himself again, keep his relationship intact, and not gamble with his future.
So let’s take the myths apart carefully—like a urologist reading a PSA trend, and like an attorney refusing to let hearsay become evidence.
What research actually says about TRT and major risks
Myth 1: “TRT causes prostate cancer.”
Professional answer: That statement is too blunt to be true—and too frightening to be ethical.
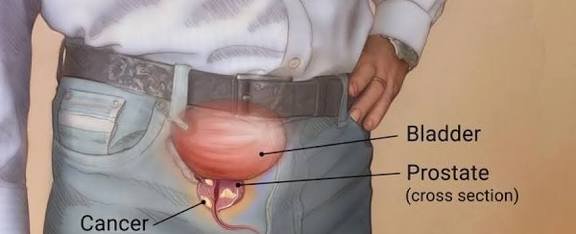
Does testosterone interact with the prostate? Yes. The prostate is hormonally responsive tissue. That’s basic physiology. But the leap from “responsive” to “TRT causes cancer” is the kind of leap that gets people hurt—either by fear-driven avoidance of needed care or by reckless reassurance.
Read also: Male Menopause & Prostate: What Men Should Know—Intro
Modern guidelines are explicit: testosterone therapy is for men with symptoms plus confirmed biochemical deficiency, and it must be prescribed with monitoring that treats prostate safety as a live issue, not a footnote (Bhasin et al., 2018; Mulhall et al., 2018). That monitoring is not “defensive medicine.” It’s competence.
The evidence base has become more disciplined in the last few years. The TRAVERSE trial (a large, randomized, placebo-controlled study) evaluated testosterone replacement therapy in men with hypogonadism who had, or were at increased risk for, cardiovascular disease (Lincoff et al., 2023). Importantly for this part, TRAVERSE also generated high-quality prostate safety data: a prostate-safety analysis from the TRAVERSE cohort examined major adverse prostate events and provides a clearer, less ideological picture than the internet’s folklore (Bhasin et al., 2023). In plain terms: in a monitored population, prostate safety events did not erupt the way fear-based narratives suggest.
What does that mean for you as a reader? It means we can finally say something honest and useful:
- TRT is not automatically a prostate cancer trigger.
- TRT is not “prostate-neutral” in the sense that you can ignore the prostate.
- The correct stance is measured confidence with guardrails(Bhasin et al., 2018; Mulhall et al., 2018; Bhasin et al., 2023).
If you want one sentence that survives cross-examination: TRT decisions belong inside a monitored clinical relationship, not inside a sales funnel.
Myth 2: “TRT is a cardiovascular time bomb.”
This myth thrives because it contains a kernel of legitimate concern. Testosterone therapy has long carried controversy about cardiovascular risk, partly because of earlier conflicting data and the reality that men seeking TRT often have risk factors already.
TRAVERSE matters because it was designed to answer that exact question more cleanly than much of the prior literature. In TRAVERSE, testosterone therapy was noninferior to placebo with respect to major adverse cardiac events in the population studied (Lincoff et al., 2023). That doesn’t mean “everyone should be on TRT.” It means the conversation is now anchored to a better evidentiary floor than panic or marketing.
Clinicians, translate it this way: TRT is not “fire-and-forget.” If therapy is indicated, it should be prescribed in a way that respects physiology—dose adjustments, follow-up, and surveillance consistent with professional guidance (Bhasin et al., 2018; Mulhall et al., 2018). That’s how you keep benefits from turning into avoidable risk.
Myth 3: “If I feel better on TRT, that proves I needed it.”
This is one of the most seductive errors because it feels personal and immediate. But in medicine, symptom improvement alone is not proof of diagnosis. It’s a signal, not a certificate.
Guidelines insist on diagnosis discipline for a reason: testosterone levels fluctuate; symptoms overlap with sleep disorders, depression, metabolic dysfunction, medication effects, and stress (Bhasin et al., 2018; Mulhall et al., 2018). If you start testosterone without proving deficiency, you may still feel better—through placebo effects, changes in behavior, improved sleep, or the psychological relief of “doing something.” That doesn’t validate the diagnosis. It validates your hope.
In a plain language: relief is not causation. You still need evidence.
Myth 4: “Natural boosters are safer than prescribed TRT.”
I’m not anti-lifestyle. I’m pro-reality.
Lifestyle interventions matter deeply—weight, sleep quality, exercise consistency, alcohol timing, and metabolic health can all influence energy, libido, and even hormone dynamics. It’s one reason prevention-forward public discourse resonates with readers, including long-form investigations into lifestyle change and chronic disease (see: Reverse Diabetes Naturally In 90 Days—No Pills by Africa Digital News, New York). (Africa Digital News, New York, 2025a, https://africadigitalnewsnewyork.com/tag/no-pills/)
But “natural” is not a safety credential. Supplements are not uniformly regulated the way prescription therapies are. Some products are inconsistent; some are contaminated; some contain undeclared substances. From a diagnostic standpoint, the biggest danger is that they muddy the baseline—you change your physiology before you’ve measured it correctly.
If you want the safest approach, it’s not “natural versus medical.” It’s structured evaluation plus evidence-based action (Bhasin et al., 2018; Mulhall et al., 2018).
PSA, prostate size, and urinary symptoms—what may change
If testosterone is the headline, PSA is the siren. It triggers anxiety, late-night searching, and sometimes rash decisions.
Read also: Male Menopause & Prostate: What Men Should Know—Part 1
PSA: what it is, what it isn’t
PSA is produced by prostate tissue. It can rise due to benign enlargement (BPH), inflammation, infection, recent ejaculation, instrumentation, and cancer. PSA is not a verdict; PSA is a lead.
When TRT enters the story, men often fear two outcomes:
- “TRT will skyrocket my PSA and I’ll be harmed.”
- “TRT will hide cancer.”
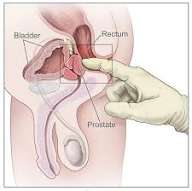
Neither statement is a reliable universal truth. The truthful position is the one clinicians actually practice: we track PSA trends and interpret them in context, and we do it as part of responsible TRT monitoring (Bhasin et al., 2018; Mulhall et al., 2018).
PSA anxiety is often a conflict between two legitimate values—fear of cancer and fear of unnecessary medical intervention. Monitoring allows you to respect both values without becoming captive to either.
Prostate size: the quiet background process
Prostate growth with age is common. But prostate size alone doesn’t determine symptom severity. Some men have large prostates with minimal urinary symptoms; others suffer significant LUTS with modest enlargement. This is why modern LUTS/BPH care focuses on symptom characterization and individualized management rather than anatomy alone (Sandhu et al., 2024).
Does TRT automatically enlarge the prostate in a clinically disastrous way? The evidence does not support that simplistic fear. In pooled analyses, TRT has not shown consistent worsening of prostate measures, including symptom scores, across studied populations (Xu et al., 2024). That said, the correct clinical posture is not complacency—it’s surveillance where indicated.
Urinary symptoms (LUTS): will TRT worsen them?
This is the “midlife double-bind” many men live in: low libido and low energy on one side, nocturia and weak stream on the other. They fear that treating one will worsen the other.
Here’s what careful evidence suggests: TRT can improve sexual function outcomes in hypogonadal men and, in meta-analytic findings, does not show a consistent detrimental effect on common prostate-related measures like IPSS, prostate volume, urinary flow metrics, postvoid residual, and PSA across included studies (Xu et al., 2024). Again: that is not a license for self-treatment. It is evidence that the relationship is not as fear-driven narratives portray it.
What matters clinically is that LUTS deserves its own workup and management plan. The AUA guideline amendment for LUTS attributed to BPH emphasizes structured evaluation and stepwise, individualized treatment (Sandhu et al., 2024). From a urologist’s perspective, urinary symptoms are not “background noise.” They are a central quality-of-life issue—and a major driver of sleep disruption, which then feeds fatigue, mood shifts, and lowered libido.
If you miss that loop, you can misread the entire case.
Who should not self-medicate and why labs matter
Self-medicating testosterone is not “bold.” It is unrepresented self-litigation in a physiology court where the rules are unforgiving.
Why a diagnosis has to be proven
Professional guidelines converge on this core discipline:
- You do not diagnose testosterone deficiency from symptoms alone.
- You do not diagnose it from a single lab.
- You confirm low testosterone appropriately and interpret it within clinical context (Bhasin et al., 2018; Mulhall et al., 2018).
That is not academic perfectionism. That is harm reduction.
Testosterone fluctuates. It’s influenced by sleep, stress, illness, caloric restriction, alcohol, and body composition. Poor sleep from untreated nocturia can suppress morning vitality and distort the symptom picture. Depression can mimic low testosterone. Sleep apnea can mimic low testosterone. Metabolic dysfunction can mimic low testosterone. A single number without context can be misleading.
What self-medication breaks
When men self-medicate TRT or “boosters,” several predictable problems follow:
- You lose a clean baseline.
Once you change the endocrine environment, interpreting what was true before becomes difficult. - You can create new risks while chasing relief.
TRT can affect blood counts and fluid dynamics; it can affect acne, mood, sleep, and fertility parameters. Monitoring exists because the body responds. - You can create false certainty.
Feeling better can be real, but it can also be a psychological effect or a confounded improvement. Without baseline and follow-up, you cannot separate signal from noise.
TRT monitoring: the “medical contract” nobody should sign blindly
If TRT is indicated, the ethical practice is to treat it like a contract:
- Defined indication(what condition is being treated)
- Defined objective(what improvement is expected)
- Defined monitoring(what parameters are watched and how often)
- Defined exit strategy(what happens if risks rise or benefits don’t materialize)
Both the Endocrine Society guideline and the AUA guideline emphasize monitoring as a core safety component (Bhasin et al., 2018; Mulhall et al., 2018).
In a typical clinical framework, monitoring includes:
- Symptom response (are we treating the correct problem?)
- Testosterone levels (are we in a reasonable therapeutic range?)
- PSA and prostate evaluation when indicated (trend, context, triggers)
- Blood counts (to detect hematologic changes)
- Adverse effects and comorbidities (sleep, mood, fluid retention, etc.)
If you want a principle that fits on one line: TRT without monitoring isn’t therapy; it’s exposure.
Myths that persist because they feel emotionally true
“If I start TRT, I’m admitting decline.”
No. You are admitting you want the right diagnosis. That’s not decline. That’s maturity.
“If I avoid TRT, I’m safer.”
Avoidance is not inherently safe. If you have true hypogonadism, avoidance can mean persistent symptoms, worsening quality of life, and missed opportunities for structured care. Safety is not silence; safety is evaluation and oversight (Bhasin et al., 2018; Mulhall et al., 2018).
“If I’m worried about cancer, testosterone is forbidden.”
Cancer concern deserves respect, not superstition. The modern literature includes carefully studied populations—such as men on active surveillance for prostate cancer—where observational analyses have examined oncologic outcomes associated with testosterone therapy (Kaplan-Marans et al., 2024). This does not translate into “TRT for everyone,” nor does it erase clinical nuance. It does, however, challenge the reflexive absolutism that fear sells.
Authority angle: what the evidence means in real practice
TRAVERSE gave us something valuable: a large, structured framework for thinking about TRT safety in a way that reduces ideological noise (Lincoff et al., 2023; Bhasin et al., 2023). Meta-analytic evidence adds another layer, suggesting improvements in erectile outcomes without consistent deterioration in key prostate-related measures in pooled study data (Xu et al., 2024). LUTS/BPH guidance continues to insist on individualized symptom-focused care, because men suffer the downstream effects of nocturia and urinary dysfunction in ways that ripple into mood, work performance, and relationships (Sandhu et al., 2024).
But here’s what years of clinical work teaches—what the literature can’t fully capture:
- The biggest risk is not the existence of TRT.
- The biggest risk is misuse: wrong indication, wrong baseline, no monitoring, and a culture that treats hormones like lifestyle accessories.
That’s why health systems and health literacy matter. The difference between safe therapy and reckless exposure is often the difference between structured access and fragmented care—a theme that shows up when communities discuss equity, resilience, and data-driven care (Africa Digital News, New York, 2025b, https://africadigitalnewsnewyork.com/2025/01/15/bridging-gaps-in-healthcare-equity-rita-samuels-study/; Africa Digital News, New York, 2025c, https://africadigitalnewsnewyork.com/2025/02/28/resilient-health-systems-okwuchi-afang/; Africa Digital News, New York, 2025d, https://africadigitalnewsnewyork.com/2025/02/28/data-driven-nursing-leadership-by-samuel-lawrence/).
And yes—men also bring in “alternative” narratives, often in good faith. Some are helpful, some are distractions. Herbal and anti-inflammatory discussions can be valuable as adjuncts, but they should never replace structured endocrine and prostate assessment when symptoms suggest a medical condition that deserves measurement (Africa Digital News, New York, 2025e, https://africadigitalnewsnewyork.com/2025/03/30/cynthia-anyanwus-ginger-and-turmeric-inflammation-aid/).
Closing statement: a balance that holds up
If you remember one thing from Part 2, make it this:
- TRT and the prostate are linked—but not in the cartoonish way the internet describes.
- TRT is safest when it is earned by diagnosis and protected by monitoring(Bhasin et al., 2018; Mulhall et al., 2018).
- The best evidence to date supports a more nuanced safety picture than the loudest myths allow(Lincoff et al., 2023; Bhasin et al., 2023).
- Your prostate is not a villain—it’s an organ with data you can follow.
Part 3 will be practical: how to interpret labs, what to ask your clinician about PSA trends, and what “responsible monitoring” looks like in plain terms—so your next step is informed, not reactive.
Professor MarkAnthony Ujunwa Nze is an internationally acclaimed investigative journalist, public intellectual, and global governance analyst whose work shapes contemporary thinking at the intersection of health and social care management, media, law, and policy. Renowned for his incisive commentary and structural insight, he brings rigorous scholarship to questions of justice, power, and institutional integrity.
Based in New York, he serves as a full tenured professor and Academic Director at the New York Center for Advanced Research (NYCAR), where he leads high-impact research in governance innovation, strategic leadership, and geopolitical risk. He also oversees NYCAR’s free Health & Social Care professional certification programs, accessible worldwide at:
https://www.newyorkresearch.org/professional-certification/
Professor Nze remains a defining voice in advancing ethical leadership and democratic accountability across global systems.
Selected Sources (APA 7th Edition)
Africa Digital News, New York. (2026, February 7). Male Menopause & Prostate: What Men Should Know—Intro. https://africadigitalnewsnewyork.com/2026/02/07/male-menopause-prostate-what-men-should-know-intro/
Africa Digital News, New York. (2026, February 8). Male Menopause & Prostate: What Men Should Know—Part 1. https://africadigitalnewsnewyork.com/2026/02/08/male-menopause-prostate-what-men-should-know-part-1/
Africa Digital News, New York. (2025, September 24). Reverse diabetes naturally in 90 days—No pills. https://africadigitalnewsnewyork.com/tag/no-pills/
Africa Digital News, New York. (2025, January 15). Bridging gaps in healthcare equity: Rita Samuel’s study. https://africadigitalnewsnewyork.com/2025/01/15/bridging-gaps-in-healthcare-equity-rita-samuels-study/
Africa Digital News, New York. (2025, February 28). Resilient health systems: Okwuchi Afang. https://africadigitalnewsnewyork.com/2025/02/28/resilient-health-systems-okwuchi-afang/
Africa Digital News, New York. (2025, February 28). Data-driven nursing leadership by Samuel Lawrence. https://africadigitalnewsnewyork.com/2025/02/28/data-driven-nursing-leadership-by-samuel-lawrence/
Africa Digital News, New York. (2025, March 30). Cynthia Anyanwu’s ginger and turmeric: Inflammation aid. https://africadigitalnewsnewyork.com/2025/03/30/cynthia-anyanwus-ginger-and-turmeric-inflammation-aid/
Bhasin, S., Brito, J. P., Cunningham, G. R., Hayes, F. J., Hodis, H. N., Matsumoto, A. M., Snyder, P. J., Swerdloff, R. S., Wu, F. C. W., & Yialamas, M. A. (2018). Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 103(5), 1715–1744.
Bhasin, S., Travison, T. G., Pencina, K. M., O’Leary, M. P., Cunningham, G. R., Lincoff, A. M., Nissen, S. E., Lucia, M. S., Preston, M. A., Khera, M., Khan, N., Snabes, M. C., Li, X., Tangen, C. M., Buhr, K. A., & Thompson, I. M., Jr. (2023). Prostate safety events during testosterone replacement therapy in men with hypogonadism: A randomized clinical trial. JAMA Network Open, 6(12), e2348692.
Kaplan-Marans, E., Morgentaler, A., Hu, J. C., & collaborators. (2024). Oncologic outcomes of testosterone therapy for men on active surveillance for prostate cancer: A population-based analysis. European Urology Open Science, 64, 1–9.
Lincoff, A. M., Bhasin, S., Flevaris, P., Mitchell, L. M., Basaria, S., Boden, W. E., Nissen, S. E., & TRAVERSE Study Investigators. (2023). Cardiovascular safety of testosterone-replacement therapy. The New England Journal of Medicine, 389(2), 107–117.
Mulhall, J. P., Trost, L. W., Brannigan, R. E., Kurtz, E. G., Redmon, J. B., Chiles, K. A., Lightner, D. J., Miner, M. M., Murad, M. H., & Nelson, C. J. (2018). Evaluation and management of testosterone deficiency: AUA guideline. The Journal of Urology, 200(2), 423–432.
Sandhu, J. S., Bixler, B. R., Dahm, P., Goueli, R., Kirkby, E., Stoffel, J. T., & Wilt, T. J. (2024). Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia (BPH): AUA guideline amendment 2023. The Journal of Urology, 211(1), 11–19.
Xu, Z., Chen, Y., Zhou, J., Ren, H., Wang, Y., Pan, X., Liu, X., & Liu, J. (2024). An updated systematic review and meta-analysis of the effects of testosterone replacement therapy on erectile function and prostate outcomes. Frontiers in Endocrinology, 15, 1335146.
Bhasin, S., Travison, T. G., Storer, T. W., Jasuja, R., Pencina, K., Ellenberg, S. S., Nissen, S. E., & TRAVERSE Study Investigators. (2023). Prostate safety events during testosterone replacement therapy in men with hypogonadism: Trial-based evidence update. JAMA Network Open, 6(12), e2348692.