“Each part of this work builds on that conviction, merging scientific rigor with narrative empathy, showing how science confirms what our ancestors already knew: that flavor is function, that culture is chemistry, and that the act of cooking is both ritual and remedy.”
An Investigative Series by Prof. MarkAnthony Nze
Investigative Journalist | Public Intellectual | Global Governance Analyst | Health & Social Care Expert | International Business/Immigration Law Professional |Strategic & Management Economist
Executive Summary
Food has always been more than nourishment; it is the body’s most intelligent technology. Long before laboratories and prescriptions, the kitchen served as the first clinic, the cook as the original clinician, and every meal as a molecular dialogue between nature and the human cell. Food as Medicine: The Secret Pharmacies in Your Kitchen reclaims that lost wisdom and reimagines it through the lens of cutting-edge science, nutrition, and global heritage. It is both a manifesto and a manual—a bridge between tradition and evidence, biology and belief, sustenance and sovereignty.
Across its twelve parts, the book dismantles the illusion that health begins in hospitals. It begins at the table. From the rediscovery of ancestral diets to the biochemistry of digestion, it reveals how every ingredient, texture, and flavor sends instructions to the body’s genes, hormones, and immune cells. It explores how inflammation—the invisible epidemic—emerges not from fate but from food systems built on ultra-processed convenience, chemical dependency, and corporate profit. Against this backdrop, the text offers a revolutionary premise: that every household can become a site of healing, and every meal, a therapeutic act.
Drawing on global research from institutions such as Harvard, the African Development Bank, the WHO, and the Institute for Functional Medicine, the book unpacks the microbiome revolution—the discovery that the gut is both an organ of digestion and a brain of emotion. It connects the molecular to the moral, showing how fermented foods, heritage grains, and natural fibers sustain the same microbial ecosystems that shape cognition, mood, and immunity. It argues that mental wellness begins in the intestines, that inflammation is the body’s rebellion against industrial food, and that longevity is a culinary practice before it is a genetic privilege.
Equally vital is the series’ exploration of food justice and the politics of health. It exposes the power structures behind modern hunger: the monopolization of seeds, the displacement of indigenous crops, and the commodification of nutrition itself. Food becomes a lens through which inequality, governance, and globalization are examined—not as abstract forces, but as biochemical realities written in blood sugar and blood pressure.
Summarily, Food as Medicine invites a paradigm shift—from treatment to prevention, from dependence to empowerment. It challenges readers to view the kitchen as a place of agency, where culinary creativity becomes clinical precision. To eat consciously is to govern biology; to cook wisely is to legislate one’s future.
The expose` closes where civilization began—in the simple, sacred act of preparing a meal. It reminds us that the true revolution in health will not come from laboratories, but from the fire, fiber, and fermentation that link our plates to our purpose. The next great medicine is already in our hands; it only waits to be cooked.
Part 1: The Forgotten Pharmacy

Where healing began — before hospitals, there was food.
Before the age of hospitals, laboratories, and pharmaceuticals, the world had only one constant healer: food. Long before medicine was professionalized or packaged into pills, the body’s first prescriptions came from the field, the forest, and the fire. In ancient Africa, Asia, and the Mediterranean, people did not speak of “nutrition science” or “diets” — they spoke of balance, harmony, and wholeness. To eat was not merely to survive; it was to participate in healing itself.
This was humanity’s original healthcare system — a pharmacy without walls, where every plant, grain, root, and leaf carried a purpose. Modern science, after centuries of detour through industrialization and commercialization, is only now rediscovering what our ancestors already knew: that the boundary between medicine and food is artificial, and that most chronic diseases of today began when we forgot to eat with reverence.
The First Healers Were Farmers
Across ancient Africa, health and nourishment were part of the same cosmology. Communities understood food as both sustenance and spirit — a moral act tied to the land. Healing was not confined to clinics; it was cultivated in gardens and harvested with intention. Millet, sorghum, fonio, baobab, hibiscus, moringa, and bitter leaf were not “superfoods” in a trendy sense — they were everyday sustenance, each contributing to strength, fertility, and longevity.
In Yoruba herbal traditions, bitter leaves were known to “wash the blood.” In East Africa, fermented milk was used to restore vitality after illness. In the Sahel, moringa leaves were crushed into porridge for nursing mothers, rich in iron and calcium. In the rainforests of Central Africa, guava leaves treated fever, while neem bark reduced inflammation. These were not superstitions; they were empirical sciences developed over centuries of observation and adaptation.
Today’s laboratories merely confirm what oral traditions preserved. African fermented foods — ogi, kenkey, togwa, injera — now draw global attention for their probiotic power, enhancing digestion and immune function. The science of the microbiome, the “gut-brain axis,” and even functional nutrition all trace their roots to this indigenous understanding: that life thrives in the balance between nourishment and nature.
The Lost Grammar of Balance
The ancients did not count calories; they counted harmony. Every meal was built on relationships — between food groups, between the body and the environment, between humanity and the divine. The idea of balance was central: hot and cold, dry and moist, bitter and sweet, solid and fluid. A healthy person was one whose meals reflected equilibrium.
The modern diet, by contrast, is designed for speed, not balance. Industrialization separated humans from the seasons, replacing cyclical abundance with constant consumption. Foods once grown locally and eaten fresh are now processed, packaged, and stripped of nutrients. Grain became refined flour; cane became sugar; oil became an industrial extract.
The transformation of food into commodity marked the beginning of nutritional amnesia. Where the village once gathered around communal meals, today’s societies eat alone, surrounded not by elders but by screens. We have replaced shared wisdom with advertising — a world where the shelf talker, not the healer, tells us what to buy.
Africa’s Forgotten Contribution
The global conversation about healthy eating is dominated by the Mediterranean Diet — celebrated for its olive oil, fish, fruits, and vegetables. Yet recent research reveals that African heritage diets, though less commercialized, are equally — if not more — nutrient-dense and ecologically sustainable.
The African food landscape offers a diversity unmatched elsewhere: grains like teff and millet, legumes like bambara groundnut, leafy greens rich in antioxidants, and fermented staples teeming with probiotics. These are not exotic curiosities; they are blueprints for sustainable nutrition.
The Mediterranean diet’s global fame owes much to its storytelling — a cultural export wrapped in European prestige. But the African diet’s anonymity is political. Centuries of colonization and food imperialism replaced native crops with export commodities. Cocoa, coffee, palm oil, and sugarcane filled ships bound for Europe, while indigenous superfoods were labeled “primitive.” The colonizer’s palate defined progress.
Today, even African urban elites aspire to imported tastes — white bread, canned soup, processed beverages — unaware that the diet of the poor in their villages might hold the very cures global nutritionists now chase. The “forgotten pharmacy” is not a metaphor; it is a historical fact erased by conquest and rebranded by commerce.
Fermentation: The Science Before Science
Among the most profound examples of ancestral genius is fermentation — a biochemical art discovered long before chemistry was named. Across Africa, fermentation was used not only to preserve but to heal. Ogi in Nigeria, togwa in Tanzania, and injera in Ethiopia all harness the power of microbes to pre-digest food, increase nutrient bioavailability, and introduce beneficial bacteria into the gut.
Modern studies show that these foods support immune function, reduce inflammation, and even regulate mood — confirming the ancient intuition that the stomach is the seat of vitality. In a world now obsessed with probiotics, kombucha, and gut health, Africa’s culinary wisdom stands as proof that innovation did not begin in laboratories but in clay pots and wooden bowls.
The Industrial Eclipse
The decline of traditional diets did not happen by accident; it was engineered. Colonial administrations and later multinational corporations reshaped African agriculture to feed global markets, not local stomachs. Policies favored cash crops over food crops, chemical fertilizers over organic compost, imports over independence.
With globalization came homogenization. Fast-food chains spread through African cities like neon weeds, replacing millet porridge with fries, palm wine with soda, and communal eating with convenience. A continent that once exported nourishment began importing illness — diabetes, hypertension, obesity — all diseases of affluence now haunting the poor.
Industrial food is efficient for profit, not for health. Its colors are artificial, its textures addictive, its shelf life longer than its nutritional value. It offers fullness without nourishment — a perfect metaphor for modern progress.
The Reawakening
Yet history is cyclical, and the forgotten pharmacy is reawakening. Across Africa, chefs, nutritionists, and community healers are reviving traditional food systems with modern insight. Urban farms grow indigenous vegetables once dismissed as “weeds.” Health campaigns promote millet and sorghum as climate-smart crops. Universities study moringa, baobab, and fonio for their nutraceutical potential.
Global health institutions now recognize that solutions to chronic disease may lie not in imported medication, but in rediscovering local knowledge. The call for “food sovereignty” — the right of people to define their own agricultural systems — has become a political movement. It is a call to reclaim both body and identity.
The Ethics of Eating
To eat is to choose — and every choice carries a moral weight. The forgotten pharmacy invites us to rethink food not just as fuel, but as philosophy. Eating locally sustains farmers. Eating seasonally respects the earth’s rhythm. Eating mindfully honors the labor of those who grow and cook.
Modern nutrition tends to moralize — to divide food into “good” and “bad.” But ancestral wisdom understood context: a meal was healthy when eaten with gratitude, balance, and community. Healing, in that sense, was social before it was chemical.
The kitchen was the most democratic clinic ever built — accessible, affordable, and communal. The same pot that fed the young nourished the old, binding generations through shared sustenance. In the act of cooking together, people practiced public health without calling it so.
Rediscovering the Healer’s Table
To reclaim food as medicine is not nostalgia; it is strategy. Chronic diseases now dominate Africa’s health burden, consuming budgets and lives. But prevention remains cheaper — and wiser — than cure. Governments invest billions in curative healthcare, yet neglect the most effective form of public health: nutrition literacy.
Imagine if schools taught not just arithmetic and grammar but the biochemistry of a balanced meal. Imagine if hospital canteens modeled dietary health instead of contradicting it. Imagine if policy makers saw every farmer as a frontline healthcare worker.
This is not idealism; it is arithmetic. One serving of bitter leaf may do more for the bloodstream than a dozen imported supplements. A diet of fresh vegetables, fermented grains, and natural oils can prevent the very diseases that pharmaceuticals merely manage.
The Return of the Original Doctor
The physician of the future, said Thomas Edison, will give no medicine but will instruct patients in the care of the human frame, diet, and prevention. Africa’s healers lived that truth centuries ago. Their clinic was the market; their medicines, the harvest.
In rediscovering this legacy, we do not reject modern medicine — we enrich it. Science gives precision to intuition, and tradition gives soul to science. When both work together, health becomes not an emergency service but a daily discipline.
Conclusion: The Pharmacy Within Reach
The forgotten pharmacy is not hidden in myth or locked in archives. It lives in the kitchen gardens of grandmothers, in the clay pots of village brewers, in the quiet resilience of traditional diets. It asks us to reimagine healing not as a transaction but as a relationship — between what we eat and who we become.
Every household can be a hospital; every meal, a prescription; every recipe, a revolution. The future of medicine may not lie in discovering new drugs, but in remembering old foods — in restoring to the table what industrialization took away.
Because long before the white coat and the stethoscope, there was a pot simmering on a fire — and in that pot, humanity’s oldest cure: nourishment with purpose.
Part 2: The Anatomy of Nutrition

Every bite is biochemistry — what you eat rewires you.
Nutrition is the most intimate form of communication between the external world and the human body. Every meal is a coded message — a biochemical dialogue that determines how cells behave, how genes express, and ultimately, how life sustains itself. To eat is not merely to feed hunger; it is to instruct biology. Each bite writes instructions in molecular language — for healing, for growth, or for decline.
At its essence, the anatomy of nutrition is the study of how food becomes self. When we consume, we do not just absorb matter; we transform it into identity — muscles, neurons, hormones, and thought. Food does not vanish in digestion; it reincarnates as us.
The Architecture of Energy
At the foundation of this transformation lie the macronutrients — carbohydrates, fats, and proteins — the triumvirate of energy and structure. These are not mere “calories,” as diet culture simplifies them, but architectural materials for the human organism.
Carbohydrates are the body’s preferred fuel, the biological equivalent of sunlight captured in molecular form. From grains, fruits, and roots, glucose enters the bloodstream and feeds every cell — but its power is double-edged. When balanced, it sustains; when abused, it corrodes. Excess sugar ignites chronic inflammation and accelerates cellular aging, a process researchers now call metabolic toxicity.
Proteins are the builders, forged from amino acids that fold into enzymes, hormones, and tissue. They are the artisans of repair, the sculptors of muscle and memory. The body continually disassembles and reassembles itself through these amino sequences — proof that we are living mosaics of what we eat.
Fats are the misunderstood geniuses of metabolism. Demonized in the industrial food era, healthy fats — from avocado, nuts, olive oil, and cold-water fish — are vital for hormone synthesis, brain function, and cellular insulation. Every nerve impulse travels through a sheath of fat; every thought depends on lipid chemistry. To fear fat is to fear the foundation of consciousness itself.
Yet, not all fats are created equal. The oils that dominate supermarket shelves — hydrogenated, refined, oxidized — distort the language of metabolism. Instead of lubricating life, they clog its pathways. Nutrition, at its deepest level, is not only about what enters the body, but about what the body can interpret without injury.
Micronutrients: The Invisible Orchestra
If macronutrients build the symphony’s stage, micronutrients — vitamins and minerals — conduct the performance. They do not provide energy directly, but they activate the enzymes and co-factors that make energy possible. In their absence, life falters in silence.
Iron carries oxygen. Zinc repairs DNA. Magnesium orchestrates muscle and nerve function. Vitamin D regulates immunity, while Vitamin B-complex fuels the nervous system and cognitive clarity. These molecules are small, but their influence is vast — they are the punctuation marks in the grammar of metabolism.
Deficiency is not always dramatic; it often whispers. Fatigue, irritability, hair loss, slow healing — these are not random inconveniences but biochemical signals. The body speaks a precise language when it lacks what it needs. Modern diets, stripped by processing and soil depletion, are rich in calories but poor in essence. We overeat and undernourish simultaneously — the paradox of plenty.
The clinical science of micronutrients reminds us that food quality is inseparable from environmental health. When soil is eroded and crops are chemically saturated, our plates inherit that impoverishment. The biology of the earth becomes the biology of its people.
Beyond the Stomach: The Body’s Nutrient Network
The traditional view of digestion begins and ends in the stomach. But modern physiology reveals a more intricate system — a network of nutrient sensing that extends from the gut to the brain, the liver, and even the microbiome.
The gut does not simply digest; it decides. Receptors along the intestinal lining detect nutrients and send hormonal signals that regulate appetite, mood, and energy expenditure. This “second brain” orchestrates the entire body’s metabolic rhythm. When we eat fiber-rich foods, it slows glucose absorption, moderating insulin response. When we consume fermented or plant-based meals, it enriches microbial diversity, reducing systemic inflammation.
Food is thus not just input; it is instruction. A single meal can alter gene expression, change immune response, and influence emotional state. The science of post-ingestive signaling — how nutrients inform the central nervous system — confirms what ancient healers already knew: the stomach is the center of both vitality and emotion.
When Food Becomes a Message of Disorder
The same molecular mechanisms that sustain life can, when distorted, accelerate decay. Poor-quality diets send chaotic signals — an overload of sugars, saturated fats, and artificial additives that confuse the body’s communication systems. Cells adapt to this noise through metabolic reprogramming, a state that leads to inflammation, insulin resistance, and cellular senescence — biological aging at the microscopic level.
In clinical terms, this is the foundation of lifestyle disease. But in moral terms, it is a crisis of disconnection — the point at which consumption forgets consequence. The tragedy of modern eating is not ignorance but indifference: we know what nourishes us, yet choose convenience over coherence.
Nutrition as Code: Rewriting the Self
Every nutrient carries information. Fatty acids influence gene transcription. Amino acids regulate neurotransmitter synthesis. Antioxidants turn off inflammatory genes. The emerging science of nutrigenomics — the study of how food interacts with DNA — reveals that diet is not destiny but dialogue.
Food choices can switch genes on or off, determining whether predispositions toward disease manifest or remain dormant. This is both liberating and daunting: every plate is a policy decision at the molecular level. When we eat, we legislate the future of our own biology.
This understanding dissolves the boundary between medicine and meal. The same biochemistry that fuels disease also fuels repair — depending on the direction of input. To eat consciously is to participate in genetic democracy.
The Body as Ecosystem
The anatomy of nutrition is not confined to human metabolism alone; it mirrors the ecology of the planet. The diversity of our diet sustains the diversity of our microbiome, which in turn sustains the diversity of life. A monotonous diet — dependent on industrial staples — starves not only individuals but ecosystems.
Every plant, root, and seed carries a unique chemical fingerprint evolved through its environment. When we consume local, seasonal, and varied foods, we ingest the rhythms of nature itself — an evolutionary alignment between environment and organism. In contrast, imported and ultra-processed diets impose metabolic uniformity, dulling both palate and physiology.
Eating, then, is an ecological act — a ritual of reciprocity between humanity and habitat. The same forces that heal the soil heal the body.
The New Science, the Old Wisdom
In clinical nutrition, the conversation often drifts toward supplementation — capsules, powders, and fortified foods. But the true revolution in nutrition is not the return to laboratories; it is the return to kitchens. Food synergy — the interaction between nutrients in whole foods — cannot be replicated synthetically. An orange offers not just vitamin C, but hundreds of phytochemicals that cooperate to create healing outcomes.
The anatomy of nutrition therefore demands humility from science: a recognition that the human body evolved in partnership with nature’s complexity, not its reduction. When we isolate a vitamin and call it “health,” we amputate its context. The orange was always wiser than the pill.
Conclusion: Eating as Enlightenment
To understand nutrition is to understand life itself — dynamic, intelligent, and interconnected. Every act of eating is an act of authorship, a rewriting of the self at the molecular level. Food carries memory: the story of the soil, the culture that cooked it, and the body that receives it.
In this anatomy, nourishment transcends the physical. It becomes an ethic — a commitment to live in harmony with the intelligence of matter. To eat consciously is to recognize that biology and morality share a table.
Every bite is biochemistry, yes — but it is also biography. We are, quite literally, what we allow to become part of us. And in that truth lies both the simplicity and the sanctity of nutrition: healing begins not in the laboratory, but in the choices we make between hunger and health, habit and awareness, ignorance and illumination.
Part 3: Inflammation — The Invisible Enemy
When the body’s alarm never turns off, healing becomes harm.
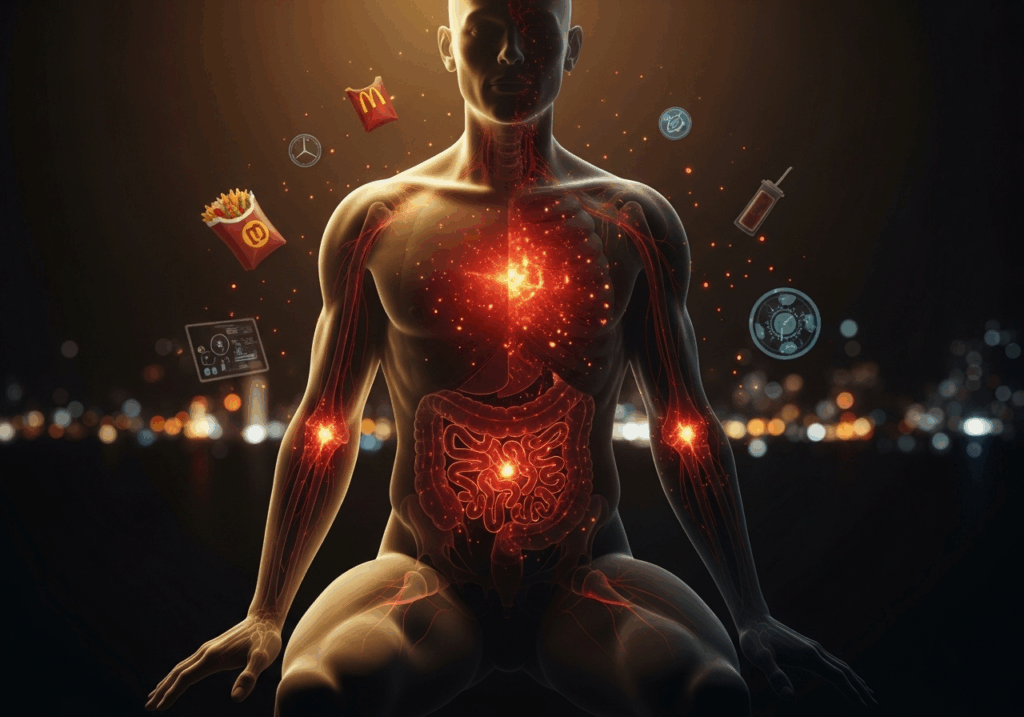
Inflammation is one of biology’s most paradoxical miracles. It is the body’s emergency response system — a siren that rushes to repair damage, kill invaders, and restore balance. Without it, even a small cut could become fatal. But when this alarm refuses to turn off, when the flames of defense smolder without cause, inflammation ceases to protect and begins to destroy. This invisible fire now fuels the world’s most chronic and costly diseases — heart attacks, diabetes, arthritis, obesity, depression, and cancer.
To understand modern illness, one must first understand inflammation — not as an isolated condition, but as a symptom of a civilization that eats, moves, and lives against its own design.
The Biology of Fire
In its acute form, inflammation is life-saving. When the body detects injury or infection, immune cells — macrophages, neutrophils, and cytokines — converge on the affected site. Blood vessels dilate, heat increases, and white blood cells flood the area. Swelling, redness, and pain are not signs of disease; they are the language of healing.
Once the threat is neutralized, anti-inflammatory agents step in to extinguish the fire. Tissues regenerate, and the system returns to equilibrium. This balance — activation followed by resolution — is the essence of health.
The problem arises when the fire never ends. Chronic inflammation is not loud; it does not manifest as fever or swelling. It burns silently, beneath the threshold of awareness, corroding tissues over years. It is inflammation unanchored from purpose — a defense without an enemy, a war without surrender.
From Healing to Harm
What turns inflammation chronic? Modern life, in almost every form, conspires to keep the immune system on high alert. The culprits are not just infections but the food we eat, the air we breathe, the stress we endure, and the sleep we deny ourselves.
Among all triggers, diet is the most insidious. The human immune system evolved to interact with food grown in soil, harvested by hand, and eaten close to its source. But the modern plate — dominated by ultra-processed foods — confuses these ancient pathways.
Refined sugars, trans fats, synthetic additives, and preservatives mimic biological invaders, provoking immune reactions that never resolve. The gut lining, once a fortress, becomes porous — a phenomenon known as “leaky gut.” Microbial fragments slip into the bloodstream, igniting systemic inflammation. The body, mistaking nourishment for threat, begins to attack itself.
This is the quiet revolution of disease: inflammation turned inward.
Ultra-Processed Foods: The Perfect Storm
Industrial foods are not just nutritionally empty; they are biochemically inflammatory. Ultra-processed products — soft drinks, instant noodles, pastries, packaged snacks — contain ingredients the body cannot interpret. Emulsifiers, artificial sweeteners, and refined oils alter the microbiome, eroding the gut’s protective barrier.
Studies now connect these foods directly to a rising wave of inflammatory bowel conditions such as IBD (Inflammatory Bowel Disease) and IBS (Irritable Bowel Syndrome). Patients who consume diets rich in ultra-processed foods exhibit overactive immune signaling, oxidative stress, and a weakened mucosal lining. What begins as digestive discomfort evolves into systemic inflammation affecting the liver, brain, and cardiovascular system.
In this way, ultra-processed diets act like slow infections — they inflame without bacteria. They do not invade the body; they convince it to destroy itself.
The Gut: Where the Battle Begins
The gut is no longer seen merely as a digestive organ; it is an immune command center. Over 70 percent of the body’s immune cells reside along its walls, constantly monitoring what passes through. The gut’s microbial population — trillions of bacteria, viruses, and fungi collectively known as the microbiome — acts as both sentinel and teacher, training the immune system to distinguish friend from foe.
When the microbiome is diverse and balanced, it produces anti-inflammatory compounds like short-chain fatty acids (SCFAs), which nourish the gut lining and suppress errant immune responses. But when this microbial diversity is destroyed — through poor diet, antibiotic misuse, or chronic stress — the equilibrium collapses. Harmful bacteria flourish, good bacteria perish, and the immune system loses its discernment.
Inflammation then escapes the gut and infiltrates the bloodstream. It reaches the brain, altering mood and cognition; the arteries, thickening their walls; and the joints, eroding cartilage. The entire body becomes an echo chamber of inflammation, responding to a problem it cannot locate.
Heart of Fire: The Cardiovascular Toll
The heart, though silent, is not spared from this biochemical war. Chronic inflammation transforms the arteries into battlefields. LDL cholesterol — the so-called “bad cholesterol” — is not dangerous on its own. The true villain is oxidized LDL, which triggers an immune response in arterial walls. White blood cells engulf these particles, forming plaques that narrow the vessels.
Inflammation thus converts repair into blockage. Over time, these plaques rupture, causing clots that lead to heart attacks and strokes. Cardiologists increasingly recognize inflammation — not cholesterol alone — as the central driver of heart disease. The modern diet, rich in refined carbs and industrial oils, supplies both the fuel and the spark for this fire.
As one medical review noted, ultra-processed foods are “the most efficient producers of inflammation known to the modern diet.” Every sugary drink and fried snack fans the flames that silently sculpt arterial walls.
Inflammation Beyond the Body: The Emotional Connection
The fire does not burn only in the blood; it smolders in the mind. The link between chronic inflammation and mental health is now undeniable. Elevated inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) are consistently found in patients with depression and anxiety.
Inflammation alters neurotransmitter metabolism, reducing serotonin and dopamine availability. It interferes with neuroplasticity — the brain’s ability to grow and adapt — leaving individuals trapped in cycles of fatigue, despair, and cognitive fog.
What we eat, therefore, does not merely feed the body; it fuels the mood. A pro-inflammatory diet not only clogs arteries but also clouds thought. Conversely, anti-inflammatory foods — omega-3 fats, turmeric, leafy greens, berries — protect neurons and stabilize emotion. Nutrition, in this sense, is psychiatry by other means.
The Anti-Inflammatory Blueprint
If inflammation is the invisible enemy, food can be the invisible cure. The anti-inflammatory diet is not a prescription but a return — a restoration of the body’s original alliance with nature. It emphasizes whole foods, unprocessed oils, fiber, and phytonutrients that modulate immune function.
Fruits and vegetables, particularly those rich in pigments — red tomatoes, orange carrots, purple cabbage — contain flavonoids and carotenoids that neutralize free radicals. Fatty fish such as sardines and salmon supply omega-3 fatty acids that suppress pro-inflammatory eicosanoids. Nuts and seeds provide magnesium and polyphenols that calm the vascular system.
Herbs and spices are the unsung pharmacists of the kitchen. Turmeric contains curcumin, a compound so potent it rivals pharmaceutical anti-inflammatories in effect. Ginger reduces cytokine activity, while garlic modulates immune cell communication. Even green tea acts as a systemic anti-inflammatory through its catechin content.
But the diet’s secret weapon is not any single food; it is the pattern — the rhythm of eating close to nature and far from factories.
Healing the Gut, Healing the System
Reversing inflammation begins with the gut. The restoration of microbial harmony requires both patience and diversity. Fermented foods such as yogurt, sauerkraut, and kefir reintroduce beneficial bacteria, while prebiotic fibers from bananas, onions, and legumes feed them.
Equally important is fasting — not starvation, but strategic rest. Intermittent fasting allows the body to clear damaged cells through a process called autophagy, reducing inflammatory burden. Sleep, too, is medicine. Chronic sleep deprivation raises cortisol and inflammatory cytokines, making rest one of the most effective anti-inflammatory therapies.
Healing is thus less about adding supplements and more about subtracting stressors — chemical, emotional, and dietary.
The Paradox of Progress
Inflammation has become the defining ailment of progress. The very technologies that promised convenience have engineered biological chaos. Our food supply is abundant yet inflammatory; our work sedentary yet stressful; our medicine advanced yet reactive.
We treat symptoms downstream while ignoring causes upstream. We prescribe pills to silence inflammation but continue feeding it at every meal. Anti-inflammatory drugs like NSAIDs can relieve pain, but they do not extinguish the fire’s source — they only mute its scream.
The true cure is preventive, not palliative. It requires a shift in culture, not chemistry — a return to the forgotten wisdom that the kitchen was humanity’s first clinic.
Conclusion: The Fire We Can Control
Inflammation is both metaphor and mechanism — a fire that can either warm or consume. It is the story of a body that remembers how to fight but forgets how to stop. And that forgetfulness, born of processed food, chronic stress, and environmental neglect, is the silent epidemic of our time.
But there is hope in reversal. Each whole meal is a truce. Each unprocessed ingredient a negotiation toward peace. The body is remarkably forgiving; it will stop burning the moment we stop feeding the flame.
The invisible enemy, after all, is not the immune system — it is our disconnection from the intelligence of the body. The cure is not hidden in laboratories but waiting on our plates, glowing in the color of real food.
When nourishment becomes mindful, the fire within does not consume — it illuminates.
Part 4: The Microbiome Revolution

Within every human, an invisible civilization governs health, emotion, and destiny.
It begins in silence — deep within the human gut, where trillions of organisms live, die, and communicate in languages science has only begun to decode. This vast ecosystem, known as the microbiome, is not a passenger within us; it is an organ in its own right — dynamic, intelligent, and indispensable. Together, these microscopic inhabitants weigh nearly as much as the human brain, yet their influence extends to every cell and system in the body. They shape immunity, regulate mood, digest nutrients, and even govern how we think.
To study the microbiome is to confront an uncomfortable truth: we are not individuals, but colonies. Human identity — physical, emotional, even cognitive — is a co-authored manuscript written in collaboration with bacteria, fungi, and archaea. The Microbiome Revolution is not just a medical discovery; it is a philosophical awakening. It forces us to reimagine the boundary between self and symbiosis — to see that health is not an isolated achievement but a negotiated harmony between species.
The Gut as an Ecosystem
Inside the complexities of the intestines, more than 100 trillion microorganisms engage in constant biochemical diplomacy. They digest what we cannot — transforming fibers into short-chain fatty acids that fuel colon cells and modulate immunity. They synthesize vitamins B and K, regulate cholesterol metabolism, and maintain the gut’s mucosal barrier — the fortress wall that separates nourishment from chaos.
In evolutionary terms, humans and microbes have been cohabiting for over 200 million years. Every bite of food, every sip of water, every breath of air has been a transaction between host and habitat. Yet, in the last century — with the rise of industrial food, antibiotics, and sterilized environments — we have dismantled this alliance. Our microbial diversity has collapsed. Diseases that were once rare — inflammatory bowel disease, obesity, allergies, autoimmune disorders — have surged, not because our genes changed, but because our microscopic partners vanished.
The modern epidemic, it turns out, is not viral or bacterial; it is ecological — a loss of microbial biodiversity inside the human gut.
The Microbial Orchestra
To understand the microbiome is to listen to the orchestra within. Every microbial species is an instrument in the symphony of health. When balanced, they produce harmony: optimal digestion, balanced mood, stable immunity. When disrupted — a condition known as dysbiosis — the music turns dissonant. Harmful microbes overgrow, beneficial ones retreat, and inflammation becomes the background noise of existence.
The consequences are staggering. Studies show that gut microbes influence everything from metabolism to mental health. They communicate with the brain through the gut–brain axis, sending chemical signals via the vagus nerve and neurotransmitters such as serotonin — of which 90% is produced in the gut. Depression, anxiety, and even neurodegenerative diseases like Parkinson’s have been linked to microbial imbalance.
In essence, the microbiome does not merely inhabit the body — it interprets it. It translates diet, stress, and environment into biochemical meaning.
Fermentation: Humanity’s First Biotechnology
Long before laboratories discovered probiotics, traditional cultures had already mastered microbial engineering through fermentation. Fermented foods — yogurt, kimchi, ogi, garri, sourdough, kombucha — were humanity’s first living medicines. Without sterile equipment or scientific jargon, our ancestors cultivated microbial allies that preserved food, enhanced nutrition, and fortified immunity.
Recent research confirms what indigenous wisdom always intuited: fermented foods are not just nourishment; they are microbiological restoration. Each spoonful delivers a microbial orchestra — Lactobacillus, Bifidobacterium, Saccharomyces — species that colonize the gut and rebalance its ecology.
A 2024 review in Nature Communications found that fermented foods increase microbial diversity and seasonal stability, buffering the gut against dietary and environmental fluctuations. In Africa, traditional ferments such as ogi (fermented maize porridge), iru (fermented locust beans), and nunu (fermented milk) contain species with powerful anti-inflammatory, antioxidant, and anti-pathogenic properties. These foods, often dismissed as “peasant staples,” may in fact hold the molecular keys to the continent’s health resilience.
Fermentation, then, is not nostalgia; it is biotechnology with a soul.
Africa’s Forgotten Microbial Heritage
Across African kitchens and marketplaces, fermentation has always been more than food science — it is cultural continuity encoded in taste. Generations have passed down microbial knowledge through clay pots and calabashes, each vessel harboring microbial lineages older than any laboratory strain.
Recent studies by Malongane, Obafemi, and colleagues have mapped the microbiome of indigenous African ferments, revealing an astonishing diversity of beneficial species absent in Western diets. These microbes not only aid digestion but also produce postbiotics — metabolic byproducts that modulate immunity and reduce oxidative stress.
In an era where global food systems homogenize diets, Africa’s fermented foods stand as a microbial archive of biodiversity. Yet this heritage is endangered. Industrial processing, chemical preservatives, and urbanization threaten to erase centuries of co-evolution between people, food, and microbes. The extinction of these microbial lineages is not just cultural loss — it is biological amnesia.
The Gut as a Second Brain
The microbiome’s influence extends beyond digestion into the deepest corridors of consciousness. Through the gut–brain axis, microbes communicate directly with neural networks, affecting emotion, memory, and cognition.
When the gut microbiome thrives, it produces serotonin, dopamine, and gamma-aminobutyric acid (GABA) — neurotransmitters that regulate happiness and calm. When it falters, inflammatory molecules cross the blood-brain barrier, altering behavior and mood. Scientists now describe depression as “inflammatory melancholy,” a sickness of both mind and microbiome.
This interdependence reframes mental health: the depressed may not always need only therapy or medication; they may also need microbial restoration. The anxious may not be mentally broken but biologically imbalanced. The mind, it turns out, sits partly in the gut.
In ancient medicine, this connection was intuitive. African, Chinese, and Ayurvedic traditions all treated digestion as a spiritual and emotional center. Today, neuroscience catches up to that wisdom.
Industrial Diets and the Microbial Extinction
Modern food is sterile — engineered for shelf life, not life itself. Pasteurization, refrigeration, and chemical additives have wiped out microbial diversity from our diets. Processed foods enter the body like empty code: caloric but devoid of living information.
The microbiome, deprived of fiber and fermented nourishment, starves. As beneficial bacteria die off, opportunistic species take over — those that feed on sugar, fats, and chemicals. These “microbial opportunists” produce toxins and inflammatory molecules, further damaging the gut barrier and immune system.
This microbial extinction mirrors the ecological collapse of the planet. As rainforests disappear above ground, microbial forests vanish within us. The gut becomes the Amazon of the body — diverse, endangered, and essential.
Fermented Foods and the Microbial Renaissance
Amid this decline, a quiet revolution brews — in kitchens, markets, and research centers. Fermented foods are making a scientific comeback, heralding a Microbial Renaissance.
In 2024, Annual Review of Microbiology documented how microbial assembly in fermented foods teaches us about ecological resilience. Each fermentation is a self-organizing system — microbes competing, cooperating, and balancing in ways that mirror natural ecosystems. Understanding these processes helps scientists design therapeutic probiotics capable of restoring diseased guts.
Moreover, traditional fermentation offers sustainable solutions to food insecurity. Fermenting grains, beans, and vegetables increases nutrient bioavailability, extends shelf life without refrigeration, and reduces food waste. It is not only health science; it is economic and ecological intelligence.
The New Pharmacology of the Gut
Medicine is now shifting from antibiotics to microbiotics — therapies that restore rather than annihilate microbial ecosystems. Fecal microbiota transplants (FMT), once controversial, have become powerful treatments for antibiotic-resistant infections. Personalized probiotic regimens are being designed to treat conditions as diverse as diabetes, eczema, and anxiety.
But the ultimate medicine remains food itself. Every fermented meal, every fiber-rich dish, is a gentle recalibration of the microbiome’s equilibrium. The gut, given the right ingredients, knows how to heal itself.
Future hospitals may prescribe meals as precisely as medications — kefir for immunity, millet beer for microbiota diversity, cassava ferment for anti-inflammatory restoration. The next frontier of healthcare may not be in pharmaceuticals, but in gastronomical therapy — a return to the microbial commons.
The Politics of the Microbiome
Behind the science lies a moral question: who controls the microbes? As the microbiome becomes commercialized, corporations race to patent probiotic strains and own microbial data. The risk is that the same logic that commodified food will now commodify life itself at its smallest scale.
Africa, with its vast microbial diversity, faces a new form of biocolonialism — the extraction not of minerals, but of microbes. Without robust bioethics and policy, indigenous fermentation cultures could become intellectual property owned abroad. The Microbiome Revolution must therefore be both scientific and sovereign. Protecting microbial heritage is as urgent as protecting rainforests or languages.
The Future of Food and the Future of Us
The microbiome teaches humility. It reminds humanity that we are ecosystems, not empires — dependent on cooperation, not domination. Health is not conquest over disease but balance within diversity.
As science deepens, one lesson endures: the fate of our microbes is the fate of our civilization. The more we sterilize, the sicker we become; the more we ferment, the more we flourish. The next agricultural revolution will not come from genetic modification but from microbial restoration — regenerating soil, food, and gut together.
If the 20th century was the era of antibiotics — the war on bacteria — the 21st century must be the era of symbiosis — the peace treaty with them. The true revolution is not technological but ecological: a return to microbial kinship.
The microbiome is not just a discovery within us; it is a mirror of the world beyond us — fragile, interdependent, alive. In saving it, we rediscover what it means to be human.
Part 5: Nature’s Insulin — Beating Blood Sugar Naturally

How the body remembers its balance, and the earth remembers the cure.
There are few molecules in the human body as powerful, misunderstood, and consequential as insulin. It is both a hormone and a herald — the biochemical messenger that whispers to our cells: “Open the gates. The sugar has arrived.” Every morsel of food, every heartbeat of energy, depends on that command. But when the message falters — when the cells stop listening — the body begins to drown in its own sweetness.
This quiet rebellion, known as insulin resistance, now defines the global epidemic of metabolic disease. More than 500 million people live with diabetes worldwide, and millions more hover in its shadow — the prediabetic state that silently erodes arteries, nerves, kidneys, and hearts. Yet this story is not merely medical; it is civilizational. Modern life — industrial food, constant stress, and sedentary routine — has rewritten human metabolism. The very systems that once protected us from famine now betray us amid abundance.
The tragedy is not that the body fails, but that it adapts — brilliantly, fatally — to an environment for which it was never designed. But nature, ever patient, still offers the antidote. For every molecule of sugar that modernity invents, the earth has already grown a counterbalance — plants, fibers, roots, and rituals that teach the body to remember its own rhythm.
This part explores that memory; how the body heals itself when fed what evolution intended — the natural insulin regulators hidden in ordinary foods.
The Evolutionary Mismatch: Why Modern Diets Break Ancient Code
Human metabolism evolved in scarcity. Our ancestors ate cyclically — feast, then fast; harvest, then hunger. The body learned thrift: store energy quickly, burn it slowly, and survive through lean times. The hormone insulin was evolution’s masterpiece in this design — it converted glucose into glycogen and fat, ensuring survival between meals.
But in the 21st century, famine never comes. Food is constant, refined, and abundant. The pancreas, built for episodic work, is now on permanent overtime. The bloodstream is flooded daily with refined carbohydrates, sweetened drinks, and ultra-processed snacks that digest faster than any natural food.
As Yale Medicine observed in 2024, “ultra-processed foods hijack the body’s hunger and satiety systems, creating an environment of perpetual eating and metabolic confusion.” These foods are engineered to be irresistible — soft, sweet, salty, and calorically dense — but biologically meaningless. They spike insulin like fireworks and leave metabolic ashes behind.
Over time, cells become numb to insulin’s message — a biochemical deafness called insulin resistance. The pancreas compensates by shouting louder, releasing more insulin, until exhaustion sets in. What follows is the collapse of metabolic dialogue: high blood sugar, high fat storage, chronic fatigue, and eventually, type 2 diabetes.
This is not just disease; it is metabolic illiteracy — the body forgetting the language of balance that nature once taught it.
The Fire Beneath the Sugar: Inflammation and Insulin Resistance
Inflammation is the invisible fire beneath nearly every chronic disease, and diabetes is no exception. According to the American Society for Nutrition (2021), chronic inflammation disrupts insulin signaling pathways, blocking glucose uptake and amplifying oxidative stress.
Each spoon of refined sugar or processed fat fuels this inflammation. The body, sensing molecular chaos, releases cytokines — immune signals that were designed to fight infections but now target the body’s own receptors. The result is a vicious cycle: inflammation worsens insulin resistance, which in turn triggers more inflammation.
The modern diet — rich in refined starches, trans fats, and chemical additives — is essentially a slow-burning inflammatory agent. By contrast, anti-inflammatory foods like berries, turmeric, ginger, leafy greens, and fatty fish calm the immune storm, restoring insulin sensitivity.
As Harvard Health (2023) noted, “a diet rich in natural anti-inflammatory compounds does more than soothe pain — it restores the molecular cooperation that defines metabolic health.”
To heal insulin resistance, one must not merely manage sugar, but extinguish inflammation — the body’s biochemical rebellion against artificial living.
The Hidden Hormone Symphony
Insulin is not an isolated actor; it performs in an orchestra of hormones — leptin, ghrelin, cortisol, glucagon, and adiponectin — that collectively regulate appetite, storage, and energy use. When one falls out of tune, the entire symphony turns discordant.
Refined foods flood the bloodstream with sugar, forcing insulin to rise sharply. Cortisol, the stress hormone, follows, ensuring glucose remains high “just in case.” Ghrelin, the hunger hormone, is amplified by sleep deprivation and emotional stress, while leptin, which signals fullness, becomes ineffective under the constant onslaught of processed fat and sugar.
This hormonal confusion is not just metabolic; it’s emotional. Cravings, fatigue, and mood swings are biochemical echoes of imbalance. Frontini et al. (2024) found that ultra-processed dietary patterns not only alter insulin response but modulate hormonal rhythms tied to mood and cognition. The same diet that feeds the body’s cravings also feeds its anxiety.
The genius of natural diets — those rooted in ancestral patterns — is that they restore harmony. Whole foods nourish the gut microbiome, stabilize cortisol, and reset leptin sensitivity. In other words, nature’s insulin is not a single compound but a hormonal ecosystem — one that thrives only in real food.
The Earth’s Insulin: Plants That Heal
Across centuries and continents, traditional diets have harbored foods that act as natural insulin sensitizers. Modern science is only beginning to validate what indigenous wisdom already knew.
- Bitter Gourd (Momordica charantia): A staple in Asian and African herbal medicine, bitter gourd contains compounds that mimic insulin’s action. It enhances glucose uptake in muscles and reduces hepatic glucose output.
- Fenugreek: Rich in soluble fiber and amino acids like 4-hydroxyisoleucine, it slows carbohydrate absorption and improves insulin response.
- Cinnamon: Beyond flavor, cinnamon increases glucose transport into cells and enhances insulin receptor activity.
- Turmeric (Curcumin): Its anti-inflammatory and antioxidant effects reduce oxidative stress, improving insulin sensitivity at the cellular level.
- Moringa: Dubbed the “miracle tree,” moringa leaves balance blood sugar and lipid profiles, providing micronutrients that modern diets lack.
- Okra: The viscous polysaccharides in okra slow sugar absorption and support gut microbial diversity, creating a protective buffer against glucose spikes.
In African traditional diets, these ingredients are not supplements; they are culture — woven into soups, teas, and stews that healed generations long before the first glucose meter.
Nurkolis et al. (2025) observed that “dietary strategies centered on whole plants, fiber, and polyphenols can improve insulin sensitivity as effectively as pharmacological agents, without side effects.”
Nature, it seems, remains the oldest and most sophisticated endocrinologist.
The Gut–Pancreas Dialogue: Microbes as Metabolic Mediators
The gut microbiome — the vast microbial community within — is the pancreas’s hidden ally. A balanced microbiome breaks down dietary fiber into short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. These molecules regulate inflammation, protect the gut barrier, and improve insulin signaling.
But ultra-processed foods, as Yale Medicine (2024) warns, devastate microbial diversity. They starve beneficial bacteria and feed inflammatory species that produce endotoxins — molecules that trigger insulin resistance.
Fermented foods such as kefir, ogi, kimchi, and fermented millet can reverse this imbalance. They reintroduce beneficial microbes that modulate glucose metabolism and dampen chronic inflammation. In this sense, fermented food is nature’s probiotic pharmacy — restoring metabolic equilibrium from the inside out.
The gut and pancreas, once thought of as separate, now appear as twin organs in metabolic communication. Heal one, and the other follows.
Fasting: The Forgotten Rhythm
Human metabolism was designed for intervals, not constancy. For millennia, humans ate according to daylight, availability, and season. Today, the clock never stops — breakfast, snacks, lunch, dinner, dessert — the pancreas works unceasingly.
Intermittent fasting restores the ancient rhythm of rest. Periods of fasting reduce insulin levels, allowing fat stores to mobilize and cells to reset their sensitivity. Studies show that even modest fasting windows (14–16 hours) improve glucose tolerance, promote autophagy (cellular renewal), and lower inflammatory markers.
More profoundly, fasting reawakens the hormonal intelligence of the body. Ghrelin stabilizes, leptin recalibrates, and cortisol quiets. The metabolic system, long trapped in noise, finally hears its own music again.
Fasting is not deprivation; it is metabolic meditation — the body’s language for balance.
The Fiber Revolution: Feeding the Inner Pharmacy
If sugar is the accelerant of disease, fiber is the brake. Soluble fiber slows glucose absorption, blunting post-meal spikes. It feeds the microbiome, lowers cholesterol, and stabilizes appetite.
Yet, the modern diet is fiber-starved. Industrial milling removes fiber for texture, and the result is metabolic mayhem. Traditional diets — rich in legumes, tubers, greens, and unrefined grains — maintain glucose harmony not by counting carbohydrates but by balancing them with their natural context.
A single cup of beans, lentils, or millet provides not only fiber but a spectrum of polyphenols that act as antioxidants and prebiotics. These foods teach the pancreas restraint and the gut resilience.
The future of metabolic health will not come from new drugs but from an old truth, the body does not crave calories; it craves complexity.
Beyond Sugar: The Psychology of Sweetness
The addiction to sugar is not only chemical; it is cultural and emotional. Sweetness has become a substitute for joy, a quick chemical comfort in an age of chronic stress. But this constant sweetness desensitizes both palate and pancreas.
The ancient palate was trained by bitterness, sourness, and complexity — flavors that signal nutrient density and microbial diversity. Bitter foods — leafy greens, herbs, fermented roots — once formed the backbone of traditional diets. They stimulate digestion, enhance liver detoxification, and regulate blood sugar.
Reintroducing bitter flavors into the diet is not an aesthetic choice; it is a neurological recalibration. It teaches the brain to associate nourishment with balance, not excess. In the war against sugar, flavor is psychology’s greatest ally.
Lifestyle as Medicine
Nutrition alone cannot rewrite insulin’s story; it must be joined by movement, sleep, and sunlight — the ancient triad of metabolic health.
Movement acts as the body’s most natural insulin sensitizer. Muscles, when active, absorb glucose independently of insulin, reducing the burden on the pancreas. Even ten minutes of walking after meals can lower blood sugar levels significantly.
Sleep deprivation, conversely, raises cortisol and inflammatory markers, impairing glucose tolerance. In one week of poor sleep, a healthy person can display prediabetic glucose profiles.
Sunlight, through vitamin D synthesis, supports pancreatic function and insulin regulation. Exposure to natural light also resets circadian rhythms, aligning hormone release with the body’s internal clock.
Each of these — movement, rest, light — is free medicine, as ancient as humanity itself. Together, they form nature’s metabolic trinity: Eat whole. Move daily. Sleep deeply.
Rethinking the Cure: From Control to Cooperation
For decades, diabetes management has focused on control — counting calories, dosing insulin, measuring glucose. But true healing does not come from domination; it comes from cooperation.
The body is not a machine to be micromanaged but a symphony to be tuned. When we align diet, rest, and rhythm with nature’s patterns, insulin sensitivity is not forced; it is restored. The pancreas remembers how to whisper, and the cells remember how to listen.
Modern medicine treats symptoms; nature retrains systems. The goal is not to suppress blood sugar but to rekindle metabolic intelligence.
The true cure is not synthetic — it is symphonic.
Conclusion: Remembering the Language of Balance
Insulin, at its core, is not a hormone of disease but of trust. It represents the body’s faith that what enters will nourish, not harm. When we feed the body in ways that betray that trust, disease follows — not as punishment, but as communication.
Nature’s insulin — found in fiber, fermented foods, plants, sunlight, and movement — is the vocabulary of metabolic peace. It does not demand control; it teaches coherence.
We are not prisoners of our blood sugar; we are participants in its rhythm. The path to balance is neither pharmaceutical nor mystical. It lies in the humble return to what we already know — that the closer our food is to the soil, the clearer its conversation with the cell.
In the end, healing insulin resistance is not about fighting the body’s chemistry; it is about remembering its music — and allowing the symphony of life to play in tune once more.
Read also: Reverse Diabetes Naturally In 90 Days—No Pills
Part 6: The Healing Plate — Designing a Medicinal Diet

When food becomes knowledge, the body remembers how to heal.
Food is the oldest form of medicine known to humankind. Long before chemistry named vitamins or laboratories measured calories, healers, mothers, and farmers already understood that nourishment was a dialogue between the body and the earth. A single meal could soothe or harm, strengthen or weaken, depending not only on what was eaten but how and when it was prepared. To eat was never a neutral act—it was participation in the rhythm of life itself.
Today, that ancient dialogue has fallen silent beneath the noise of industrial food, convenience, and excess. The modern plate, polished and packaged, is abundant in quantity but impoverished in intelligence. It feeds the tongue but starves the cell. We have replaced the art of nourishment with the science of consumption, and the consequence is written in the statistics of chronic disease—diabetes, hypertension, fatigue, anxiety—conditions that rise not from scarcity but from misalignment.
The healing plate restores this lost grammar of health. It is not a diet, nor a list of forbidden pleasures. It is a philosophy of eating that returns food to its rightful place—as the bridge between biology and being, chemistry and consciousness, pleasure and preservation. To design such a plate is to recognize that every meal is a molecular message, a chemical conversation with the body’s deepest systems.
The Chemistry of Nourishment
The human body is a living laboratory, powered by millions of chemical reactions that never rest. Proteins, fats, carbohydrates, vitamins, and minerals are not abstract terms from textbooks—they are the vocabulary of vitality. Each molecule plays its role in maintaining the architecture of life: repairing tissues, generating energy, balancing hormones, and guarding against decay.
When this molecular conversation flows freely, the body thrives. But when diet introduces confusion—too much sugar, too few minerals, too many synthetic additives—the language of life becomes garbled. Metabolic pathways misfire, hormones lose rhythm, and inflammation begins to whisper in the background.
The secret to designing a healing plate is fluency: learning to speak the body’s biochemical language. It means giving the cells the materials they understand—unrefined, complete, alive—and removing the impostors that mimic nourishment while delivering none.
True nutrition is not about abundance; it is about alignment. The goal is not to eat more, but to eat right enough—to eat in harmony with the body’s design and the planet’s cycles.
The Foundation: Macronutrients as Architecture
Every structure needs its building blocks, and in the human body, these are the macronutrients: carbohydrates, proteins, and fats. They do not merely fill us—they form us.
Carbohydrates are the body’s most immediate source of energy, but they must be treated with discipline. In their natural state—embedded in fiber, as in whole grains, legumes, or root vegetables—they release glucose slowly, nourishing both muscle and mind without chaos. But when stripped of fiber and minerals, as in white flour and refined sugar, they flood the bloodstream with energy the body cannot safely store. The pancreas responds with alarm, insulin surges, and over time the rhythm of metabolism collapses into resistance and fatigue.
Proteins are the sculptors of form. Every muscle, enzyme, antibody, and neurotransmitter begins as a strand of amino acids. Yet protein’s power lies not only in quantity but in diversity. A healing plate borrows from ancestral wisdom: grains paired with legumes, seeds combined with roots. Each pairing completes the other’s amino acid profile, creating a harmony industrial diets have forgotten.
Fats, long demonized, are the body’s quiet architects of thought and emotion. They build cell membranes, modulate inflammation, and compose the brain’s architecture. Healthy fats—olive oil, avocado, coconut, groundnuts, walnuts, fish—are not luxuries; they are necessities. They anchor hormonal balance and sustain calm cognition. Processed fats, on the other hand, deform cell membranes, blocking communication between cells. The difference between vitality and exhaustion often lies in the type of fat on the plate.
The body does not crave extremes—it seeks balance. Too much carbohydrate inflames; too little fat destabilizes; too little protein weakens. The healing plate honors proportion: half plants, a quarter protein, a quarter whole grains or roots, and a measure of natural fat to bind them together in chemistry and meaning.
The Hidden Symphony: Micronutrients and Mineral Intelligence
If macronutrients are the architecture, micronutrients are the engineers. They work silently, unseen, yet their absence is catastrophic. Magnesium keeps the heart in rhythm. Zinc repairs wounds and supports immunity. Selenium defends DNA from oxidative harm. Vitamin D synchronizes mood with sunlight. Iron breathes oxygen into every cell.
Modern agriculture, obsessed with yield, has stripped the soil—and thus our food—of these invisible allies. The result is a world that eats too much yet remains malnourished. Micronutrient deficiency does not announce itself with hunger; it hides behind fatigue, irritability, and chronic illness.
To restore the body’s mineral intelligence, the healing plate emphasizes diversity of source. Each color of plant, each type of nut, seed, or grain contributes a different mineral signature. A plate of monochrome food, no matter how abundant, cannot match the spectrum of nutrients in a rainbow of natural produce. Green vegetables whisper calcium and magnesium; orange and yellow fruits deliver carotenoids; purple and blue foods bring anthocyanins, the pigments of protection.
The wisdom is simple: eat with color, eat with curiosity, eat with gratitude.
Hormonal Harmony: The Endocrine Dialogue
Every meal speaks directly to the body’s hormonal system. Food is not passive—it instructs. Carbohydrates summon insulin, fats modulate estrogen and testosterone, protein signals growth and repair, and minerals guide thyroid and adrenal function.
When the diet is erratic, hormones lose rhythm. Constant snacking and refined sugars force insulin to rise and fall like a storm. Skipping meals or eating under stress elevates cortisol, the stress hormone, which in turn disrupts sleep, mood, and weight balance. Artificial additives confuse hormonal receptors, imitating signals that should never have been sent.
The healing plate restores this inner dialogue through rhythm and respect. Meals are eaten at steady times, not as afterthoughts but as rituals. Sugar gives way to natural sweetness—fruit, honey, or nothing at all. Fats become allies again, supporting hormone production rather than clogging it. Protein stabilizes energy between meals.
When food is rhythmical, hormones become music once more. The body learns again how to rest, repair, and reproduce—not through medication, but through order.
The Architecture of Youth: Cellular Renewal through Food
Aging is often misunderstood. It is not merely the accumulation of years, but the gradual decline of cellular communication. Inside each tissue, cells renew, repair, or retire. The rate at which they do so determines the pace of aging. Diet plays a decisive role in this invisible clock.
Certain foods accelerate decay: refined sugars, hydrogenated oils, and chemical additives flood the body with free radicals—unstable molecules that attack cell structures. Over time, the body fills with senescent cells—old, inflamed, half-dead cells that neither die nor heal. They release toxins that agesurrounding tissues.
Yet other foods do the opposite. Cruciferous vegetables like broccoli, cabbage, and kale activate detoxification enzymes that clear cellular waste. Berries, onions, turmeric, garlic, and green tea contain polyphenols that repair DNA and reduce oxidative damage. Sulfur-rich vegetables feed the liver’s ability to cleanse the bloodstream. Omega-3 fats soothe inflammation and promote new cell membranes.
A healing plate, eaten consistently, teaches cells to renew rather than rust. It cannot halt time, but it can alter its tone—transforming decline into grace.
Rhythm, Timing, and the Science of Eating
What we eat matters, but so does when. Human metabolism is bound to the cycles of light and darkness, wake and rest. Eating with the sun—larger meals earlier, lighter ones later—aligns digestion with circadian biology.
When food arrives too late, digestion competes with sleep. Blood sugar remains high through the night, hormones falter, and rest becomes shallow. A morning rich in fiber and protein steadies energy. Lunch provides fuel for productivity. Dinner should be peace, not indulgence—a whisper rather than a shout.
This rhythmic eating, sometimes called chrononutrition, allows the digestive organs to work when they are meant to and to rest when they must. It is not a rule of deprivation but a restoration of rhythm.
The Mind as the First Ingredient
Digestion begins not in the stomach, but in the mind. The sight, smell, and thought of food trigger enzymes, saliva, and stomach acid. Yet most people now eat while distracted—scrolling, rushing, arguing. The nervous system remains in a state of tension, and digestion shuts down.
To eat mindfully is to return to the original sacrament of nourishment. It means slowing down, chewing deliberately, breathing between bites. It means gratitude—not as a gesture of faith, but as a signal to the body that it is safe to receive.
When the mind is calm, digestion deepens. Nutrients absorb more efficiently. The immune system rests. The body interprets food as a gift, not a threat.
The healing plate, therefore, is not complete without stillness.
Ecology as Health
Every plate begins in the soil. If the earth is sick, the eater will be too. Modern food systems, with their pesticides, plastics, and monocultures, have not only poisoned ecosystems—they have hollowed out nutrition itself. The healing plate is therefore an ecological statement as much as a medical one.
Choosing food grown locally and seasonally restores nutrient integrity. Supporting regenerative farming rebuilds the minerals in the soil, which return to the plants and, eventually, to us. A tomato grown in rich, living soil is not the same as one raised on synthetic fertilizer. One carries life; the other carries residue.
To eat consciously is to take responsibility for the web of life that feeds us. Every purchase, every meal, either heals or harms the earth—and by extension, ourselves. The health of soil, plant, and person is one continuous ecosystem.
The Return of Ancestral Wisdom
Long before laboratories confirmed it, ancient cultures already knew the principles of the healing plate. African stews, Mediterranean spreads, Asian broths—all were rooted in balance, fermentation, and seasonality. Millet paired with beans, sorghum fermented in clay, greens cooked with oil and spice—all of these traditions achieved biochemical harmony by intuition.
Modern nutrition is rediscovering what was once common sense: diversity, moderation, and freshness sustain more than the body—they sustain civilization itself. In the past, food connected families and generations; today it must reconnect science with soul. The future of medicine may well depend on remembering the kitchens of the past.
Designing the Modern Healing Plate
To design a modern healing plate, one begins not with restriction, but with intention. Food should be whole, colorful, and alive. The plate should represent the seasons—root vegetables and grains in cooler months, fresh fruits and greens in warmer ones.
Half of the plate belongs to plants: vegetables, legumes, and fruits. A quarter is protein, chosen for quality rather than quantity. The final quarter holds complex carbohydrates—brown rice, quinoa, millet, yam, or sweet potato. Fats enter not as an afterthought but as a binding principle, balancing flavor and function.
Water remains the only true drink of health, and fermented foods—yogurt, kimchi, kefir, ogi—should appear daily, feeding the microbiome that governs digestion and immunity.
Eating thus becomes art again—an act of creation, not consumption.
The Philosophy of the Healing Plate
To eat well is to live consciously. The healing plate is less a meal plan than a moral compass. It asks us to consider the origin of our food, the rhythm of our hunger, and the purpose of our nourishment. It reminds us that food is not only chemistry but relationship: between soil and soul, sunlight and cell, hunger and gratitude.
Every meal is a vote—for health or for decay, for nature or for neglect. To design a medicinal diet is to reclaim responsibility for one’s existence, one bite at a time.
The healing plate does not preach austerity; it celebrates balance. It honors pleasure, but without excess. It makes science beautiful again, and beauty scientific. It is both discipline and delight, a ritual of remembering that we are sustained not by industry, but by intimacy—with the land, with time, with the miracle of being alive.
When food and awareness reunite, the body does not merely survive—it awakens. The heart steadies, the skin glows, the mind clears, and the old fatigue fades. Because true nourishment is not about eating to live longer, but about eating to live rightly. In that rightness, medicine dissolves, and the body begins to speak again the forgotten language of healing.
Part 7: The Gut-Brain Axis — How the Stomach Speaks to the Mind
The body thinks, the mind digests, and between them lies the gut—the hidden seat of emotion, intuition, and health.
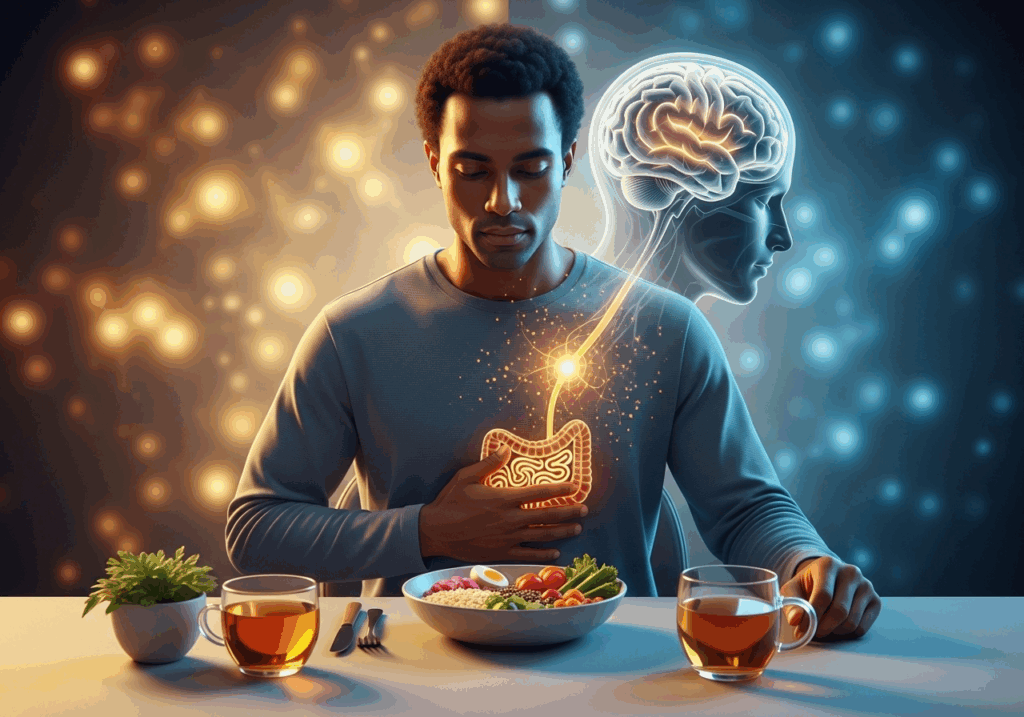
For centuries, medicine treated the body as a machine and the mind as a mystery. The stomach was a site of digestion, the brain a citadel of thought, and the two, it seemed, had little to say to one another. But biology has now revealed what ancient wisdom always intuited: the gut and the brain are not separate kingdoms—they are twin halves of the same nervous system, communicating in whispers of hormones, microbes, and memory.
Every mood, every craving, every impulse passes through this invisible network. When the stomach is inflamed, the mind grows anxious; when the microbiome thrives, joy feels more accessible. In every language, this truth survives in metaphor—we speak of “gut feelings,” “nauseating fear,” “sickening grief.” Modern neuroscience has simply confirmed what the body has always known: emotion begins in the gut.
The gut-brain axis is more than a biological curiosity; it is the future of holistic health. Understanding it transforms how we treat not only digestion, but depression; not only appetite, but awareness. The stomach, it turns out, is not just a vessel—it is a second brain.
The Hidden Brain Beneath the Diaphragm
Embedded within the walls of the intestines lies a vast neural network known as the enteric nervous system. Containing over 100 million neurons—more than the spinal cord—it controls digestion, movement, secretion, and immune response. This “second brain” operates semi-independently but remains in constant communication with the brain above via the vagus nerve, a superhighway of bi-directional signals that connects gut, heart, lungs, and mind.
This communication is not symbolic but chemical. The gut produces more than 90% of the body’s serotonin, the neurotransmitter of happiness and calm. It also synthesizes dopamine, GABA, and other neurochemicals traditionally associated with the brain. When the gut’s environment—its microbial balance, nutrient flow, and inflammation level—is disturbed, these messages change. The result can manifest as anxiety, depression, irritability, or chronic fatigue.
We are not only what we eat; we are what our bacteria become.
Microbes as Messengers
The human gut is home to trillions of microorganisms—bacteria, fungi, and archaea—forming what scientists now call the microbiome. This inner ecosystem is as complex as a rainforest, with hundreds of species coexisting in delicate equilibrium. These microbes are not passive passengers; they are active participants in physiology. They digest fiber into short-chain fatty acids that nourish colon cells, train the immune system to distinguish friend from foe, and even produce neurotransmitters that shape emotion and cognition.
A balanced microbiome is like a well-governed city: diverse, stable, self-regulating. But modern life—antibiotics, processed food, chronic stress, and lack of sleep—has turned many guts into metabolic wastelands. The disappearance of beneficial bacteria allows harmful strains to dominate, releasing endotoxins that leak through the gut wall and trigger systemic inflammation. This “leaky gut” becomes a silent source of chaos in the brain, contributing to mood disorders, memory decline, and neurodegenerative disease.
Healing the mind, therefore, often begins with feeding the microbes.
The Diet of Connection
The foods that restore gut balance are not exotic or expensive; they are the simple, ancestral ingredients that industrialization replaced with plastic and powder. A medicinal diet for the gut-brain axis emphasizes prebiotics—fibers that feed beneficial bacteria—and probiotics—living cultures that replenish them.
Prebiotics thrive in vegetables, fruits, legumes, and whole grains: garlic, onions, asparagus, oats, and bananas. Probiotics arrive through fermented foods: yogurt, kefir, sauerkraut, ogi, kimchi, or traditional African beverages like kunu and palm wine in moderation. These living foods carry bacteria that colonize the gut and reawaken dormant microbial networks.
When the microbiome revives, it begins producing butyrate, acetate, and propionate—short-chain fatty acids that reduce inflammation, fortify the gut lining, and calm the nervous system. People who eat diverse, fiber-rich diets often report more stable moods, sharper focus, and deeper sleep—not because of magic, but because their microbes have regained their voice.
The gut does not simply digest food; it digests experience.
Inflammation, the Silent Saboteur
Inflammation is the body’s language of distress. In small doses, it heals wounds and fights infection. But when it becomes chronic, it corrodes everything it touches—from blood vessels to neurons. The gut is both the origin and the victim of this fire. Processed food, sugar, alcohol, and artificial additives inflame the intestinal walls, weakening the barrier that separates the digestive tract from the bloodstream.
Through this damaged barrier—known as increased intestinal permeability—bacterial fragments and toxins seep into circulation, prompting the immune system to wage war against phantom invaders. The resulting cytokine storm travels upward to the brain, where it dulls neurotransmission, disrupts sleep, and clouds emotion.
Modern neuroscience calls this neuroinflammation—a silent contributor to depression, brain fog, and even Alzheimer’s disease. The mind becomes foggy not because it lacks willpower, but because the body beneath it burns unseen.
To soothe the brain, one must cool the gut. Anti-inflammatory foods—leafy greens, berries, turmeric, ginger, olive oil, and omega-3 fats—are not merely dietary trends; they are medicine. When inflammation subsides, clarity returns, not as optimism but as chemistry restored.
Stress, the Disruptor of Digestion
No system suffers more under stress than the digestive tract. When the brain perceives threat, real or imagined, it diverts blood away from the intestines toward the muscles and heart—a perfect response for escaping predators, disastrous for modern living. Chronic stress freezes peristalsis, suppresses stomach acid, and alters gut microbiota. Constipation, bloating, reflux, and irritable bowel syndrome often trace back to relentless cortisol rather than poor diet alone.
The gut and brain mirror each other. An anxious mind tightens the stomach; a distressed gut amplifies anxiety. This feedback loop, if left unbroken, erodes both.
The antidote lies not in pills but in rhythm. Deep breathing, mindful eating, yoga, meditation, prayer, and regular rest activate the parasympathetic nervous system—the “rest and digest” mode. When peace enters the mind, digestion resumes its natural grace. Stress management is not an accessory to nutrition; it is nutrition for the nervous system.
Mood, Memory, and the Microbial Mind
Scientific studies increasingly link gut health with emotional regulation. People with diverse gut flora score higher on measures of happiness and resilience. Those with depleted microbiomes are more prone to anxiety, insomnia, and depression. The mechanism is biochemical: gut bacteria manufacture neurotransmitters like serotonin, dopamine, and GABA, and modulate the expression of brain-derived neurotrophic factor (BDNF), a protein critical for memory and learning.
But the relationship is reciprocal. Thoughts and emotions also shape microbial composition. Chronic fear alters bile flow and intestinal pH, creating an environment that favors pathogenic bacteria. Optimism, laughter, and gratitude, by contrast, stimulate vagal tone and promote microbial diversity.
The conclusion is radical: joy has a biology, and bacteria have psychology.
The Gut as the First Immune Organ
Nearly 70% of the immune system resides in the gut-associated lymphoid tissue (GALT). Every mouthful of food introduces new microbes and molecules that must be identified as safe or harmful. The immune system learns tolerance here, distinguishing nutrition from threat.
When the microbiome is healthy, this immune training is calm and precise. But when diversity collapses, the immune system becomes trigger-happy, attacking not only invaders but the self. Autoimmune diseases—such as Crohn’s, lupus, and rheumatoid arthritis—often begin in this miseducation of the gut.
Healing the immune system, therefore, requires rebuilding the microbial classroom. Fiber, fermented foods, and polyphenol-rich plants serve as textbooks for immune intelligence. The lesson is simple but profound: immunity begins with digestion, not defense.
Sleep, Appetite, and the Gut Clock
The gut has its own circadian rhythm. Microbial populations fluctuate through the day, influenced by light exposure, meal timing, and rest. Late-night eating confuses this cycle, leading to erratic digestion and poor sleep. A disrupted microbiome, in turn, alters melatonin and ghrelin—the hormones that govern rest and hunger.
The result is the modern triad of imbalance: insomnia, cravings, and fatigue. Restorative sleep is not only psychological; it is bacterial. Regular meal times, early dinners, and nightly fasting periods allow the microbiome to regenerate. Each night, trillions of microbes perform housekeeping—digesting, detoxifying, recalibrating. To eat mindfully by day is to dream deeply by night.
The Taste of Emotion
Taste itself is emotional. The palate remembers what the heart cannot. Sweetness comforts, bitterness cleanses, sourness awakens, salt grounds. Each flavor speaks a physiological dialect tied to emotion. Traditional medicine systems like Ayurveda and Chinese herbalism recognized this correspondence: bitterness for anger, sourness for stagnation, sweetness for sadness.
Modern nutrition now confirms these intuitions. Cravings are often compensations for biochemical imbalance. Sugar addiction mirrors serotonin deficiency; salt cravings accompany adrenal fatigue; desire for fried food masks low dopamine. To heal the diet is therefore to translate the emotions beneath it. The question is not why am I eating this? but what am I trying to feel?
When emotion is processed consciously, appetite becomes an ally, not an addiction.
The Language of Healing
The gut-brain axis teaches that healing cannot be compartmentalized. Food, mood, thought, and immunity are threads of one tapestry. A meal that soothes the gut calms the mind; a quiet mind strengthens digestion. The stomach listens to what the brain believes, and the brain listens to what the stomach feels.
Designing a diet for this axis is not about rigid rules but about respect for rhythm, diversity, and awareness. It means slowing down, choosing real foods, hydrating deeply, and honoring the quiet intelligence that lives in every cell and bacterium. It also means acknowledging that modern illness often arises from forgetting this relationship—treating the body as machine rather than ecosystem.
To restore balance, one must feed the whole being: the microbes, the nerves, the breath, and the thought.
Toward a New Medicine of Connection
The emerging field of psychobiotics—the study of microbes that influence mental health—signals a revolution in how we understand well-being. Future antidepressants may be found not in pharmaceuticals but in fermented foods. The next great therapy for stress may involve restoring the microbiome rather than suppressing symptoms.
But the principle is ancient. When the African healer offered fermented millet to a grieving family, when the Mediterranean diet combined olive oil, garlic, and herbs, when Chinese medicine prescribed soups for sadness—they were practicing psychobiology before the term existed. Their intuition was empirical: to heal the mind, feed the gut.
Modern science has finally caught up with ancestral wisdom. The gut-brain axis is not new; it is newly remembered.
The Philosophy of Wholeness
Health is not the absence of disease; it is the presence of harmony. The gut-brain axis is the most eloquent expression of this truth. It reminds us that no thought is purely mental, no digestion purely physical. Each emotion shapes chemistry, and each meal shapes consciousness.
To nourish the gut is to polish the mirror of the mind. To feed the mind with peace is to heal the stomach. Between hunger and happiness lies a single organ of connection, pulsing quietly beneath the ribs, holding the wisdom of both evolution and emotion.
When we listen to that organ—not as an afterthought but as a guide—we rediscover the unity that medicine once lost: that food is feeling, that thought is digestion, and that every act of eating is also an act of thinking.
The gut speaks in sensations: warmth, discomfort, fullness, longing. The mind translates these sensations into stories. Healing begins when the stories and the sensations finally agree—when the body and the mind say the same thing at the same time: I am at peace.
And in that moment, both digestion and consciousness begin again.
Part 8: The Hormone Highway — The Invisible Currents of Life
When hormones flow in harmony, the body becomes an orchestra. When they fall out of rhythm, even the strongest instrument plays off-key.
The human body is not powered by muscle or mind alone—it runs on an invisible river of messages. These messages are the hormones: chemical couriers that move through blood like whispers, linking organ to organ, mood to metabolism, hunger to thought. They are the quiet architects of growth, fertility, sleep, and even self-perception. Without them, the body would be an uncoordinated crowd of organs, each acting without knowing what the other feels.
To understand health is, therefore, to understand hormones. They are not merely reproductive signals; they are the grammar of life’s balance. Every heartbeat, every breath, every emotion is orchestrated by these messengers. The endocrine system—the network of glands that secrete them—is not a machine but a highway of meaning, carrying instructions that translate nutrition into vitality, rest into renewal, and stress into survival.
Modern living, however, has turned this highway into a battlefield. Processed food, sleep deprivation, environmental toxins, and chronic stress have clogged the lanes, scrambled the signals, and thrown the body’s natural communication into chaos. Yet within that chaos lies an opportunity—to rediscover how the right foods, habits, and rhythms can repair the traffic of life itself.
The hormone highway is not a metaphor. It is a living network through which energy, reproduction, immunity, and emotion travel. To balance it is to restore the conversation between the brain, the gut, the glands, and the spirit.
The Architecture of the Endocrine System
The body’s endocrine system is a network of precision. It includes the pituitary gland—the conductor in the brain that coordinates the orchestra. It commands the thyroid to regulate energy, the adrenals to handle stress, the pancreas to balance sugar, and the reproductive organs to sustain continuity.
Hormones are molecules of power, yet they act in micrograms. A few drops too few, and the body slows into fatigue; a few drops too many, and it races toward anxiety or disease. Their harmony depends on feedback—signals that move in loops. The brain monitors hormone levels constantly, adjusting production to maintain equilibrium.
This delicate system, however, depends on raw materials: fats, amino acids, vitamins, and minerals. Without cholesterol, the body cannot synthesize estrogen, progesterone, or testosterone. Without zinc or vitamin B6, thyroid function falters. Without iodine, metabolism dulls. Without sleep, even insulin—the hormone of energy—loses discipline.
Hormonal health, therefore, begins with biochemical literacy. The body does not produce balance out of willpower; it requires nourishment that speaks the language of its glands.
The Dance of the Big Four
Among the hundreds of hormones that guide the body, four dominate daily life: insulin, cortisol, thyroid hormones, and sex hormones (estrogen, progesterone, and testosterone). They do not act alone; they perform as a quartet, each influencing the rhythm of the other.
Insulin, secreted by the pancreas, governs energy distribution. It decides whether glucose becomes fuel or fat. When diet leans heavily on refined carbohydrates and sugars, insulin floods the bloodstream, storing excess energy in fat cells. Over time, the cells stop responding—creating insulin resistance, a quiet epidemic that leads not only to diabetes but to fatigue, cravings, and brain fog.
Cortisol, the stress hormone, is the body’s emergency siren. In short bursts, it saves lives—raising blood sugar, sharpening focus, heightening alertness. But when stress becomes constant, cortisol refuses to step down. Chronically elevated, it suppresses immunity, weakens muscles, and distorts sleep. It also interferes with insulin, perpetuating a vicious cycle of stress and sugar.
Thyroid hormones—T3 and T4—control metabolic tempo. They determine how quickly cells burn fuel, how warm the body feels, and how sharp the mind remains. Thyroid imbalance manifests in extremes: sluggishness, weight fluctuation, dry skin, or restlessness. The gland itself depends on iodine, selenium, and iron—nutrients often missing in depleted soils and processed foods.
Finally, sex hormones—estrogen, progesterone, and testosterone—shape far more than reproduction. They influence mood, motivation, bone strength, and heart health. In both men and women, they are the chemistry of vitality. Yet their harmony is fragile, disrupted by stress, pollution, synthetic chemicals, and poor diet.
To heal the body is to invite these four to dance again—not in competition, but in rhythm.
Food as the First Hormone Regulator
Hormones are born from nutrients. Every gland draws its strength from the pantry. The fats we eat become raw material for estrogen and testosterone. Amino acids from protein fuel thyroid hormones and neurotransmitters. Micronutrients act as co-factors—tiny keys that unlock hormonal pathways.
A hormone-friendly diet begins not with deprivation but with precision:
- Healthy fats from avocados, olive oil, nuts, and fish rebuild cellular membranes, enabling hormones to dock properly on their receptors.
- Fiber from vegetables and whole grains supports the liver in detoxifying excess hormones, especially estrogen.
- Protein stabilizes blood sugar, preventing insulin spikes.
- Magnesium, zinc, and selenium fine-tune the production of thyroid and sex hormones.
- Cruciferous vegetables—broccoli, cabbage, kale—contain compounds that regulate estrogen metabolism, reducing risk of hormonal cancers.
- Fermented foods nurture the gut microbiome, which influences the breakdown and recycling of hormones.
The body’s biochemistry is democratic. It rewards consistency, not perfection. Every meal either adds friction to the hormone highway or clears the lanes.
The Stress Loop
No hormone shapes modern life more than cortisol. It is the biology of worry, the chemistry of survival. But unlike ancient humans, who fought wild animals and rested afterward, today’s cortisol never finds an ending. It rises with alarm clocks and deadlines, traffic and screens, caffeine and fear.
Cortisol’s mission is simple: to keep the body alert by releasing glucose for immediate energy. But when its signal stays on, insulin must intervene to lower that glucose. The tug-of-war exhausts both hormones, leading to energy crashes, cravings for sugar, and emotional volatility.
This biochemical stress loop is the hidden root of many disorders once dismissed as “lifestyle issues.” Chronic fatigue, anxiety, insomnia, and weight gain are not failures of will—they are the physiology of imbalance.
The antidote is rhythm. Meditation, deep breathing, yoga, and laughter all lower cortisol levels measurably. So does nature—sunlight on skin, soil underfoot, silence between thoughts. Even simple habits like keeping regular meal times and seven hours of uninterrupted sleep restore the body’s hormonal dialogue.
Stress is inevitable, but its damage is optional.
The Thyroid — The Body’s Thermostat
If cortisol is the body’s emergency light, the thyroid is its pilot flame. It burns quietly in the throat, regulating how fast or slow every cell performs its task. The thyroid does not work alone—it listens to the brain’s pituitary signals and responds based on available nutrients.
When the thyroid slows, energy falters, the pulse softens, and metabolism drifts into lethargy. When it races, anxiety, heat, and restlessness take over. This gland’s stability depends on iodine, selenium, zinc, and iron—minerals often stripped from modern diets by industrial processing.
Healing the thyroid means nourishing it. Sea vegetables, nuts, seeds, legumes, and clean sources of protein restore the trace minerals that keep its flame steady. Avoiding endocrine-disrupting chemicals in plastics, pesticides, and cosmetics protects it from overload.
The thyroid is the body’s quiet clock. When it keeps time, everything else follows.
The Language of Reproduction
Estrogen, progesterone, and testosterone are not confined to reproduction—they orchestrate the symphony of life’s vigor. They influence memory, heart rhythm, muscle tone, and even the sparkle in one’s eyes. Their balance, however, is easily disturbed.
Excess estrogen—often caused by exposure to xenoestrogens (synthetic chemicals in plastics, cosmetics, and pesticides)—can cause fatigue, mood swings, and weight gain. Low progesterone may lead to anxiety and insomnia. In men, declining testosterone is linked not only to libido loss but to decreased motivation and cognitive sharpness.
Food and lifestyle shape these hormones profoundly. Regular physical activity raises testosterone and growth hormone naturally. Adequate sleep boosts progesterone and melatonin. Cruciferous vegetables and high-fiber diets help eliminate excess estrogen. Avoiding refined sugar, alcohol, and processed meats protects the liver—the organ responsible for hormonal balance.
The body does not age because hormones decline; hormones decline because the body forgets how to communicate. The task of wellness is to restore that dialogue.
Micronutrients — The Unsung Heroes
Hormones are only as intelligent as their environment. Micronutrients function as translators—bridging the gap between nutrition and endocrine precision.
- Magnesium calms the nervous system, moderates cortisol, and supports estrogen detoxification.
- Vitamin D acts as both hormone and hormone modulator, influencing immunity, mood, and insulin.
- B vitamins govern energy production and neurotransmitter synthesis.
- Selenium and zinc enable the thyroid to convert its inactive hormone (T4) into the active form (T3).
- Chromium and vanadium enhance insulin sensitivity, stabilizing energy levels.
Deficiency in any of these creates a domino effect: the thyroid slows, cortisol spikes, insulin resists, and mood deteriorates. Supplementation can help, but the truest medicine remains food—diverse, whole, unprocessed.
Reprogramming the Rhythm
Hormones do not respond to intensity; they respond to consistency. Healing the endocrine system requires reintroducing rhythm into modern chaos.
- Eat at regular intervals to stabilize insulin and cortisol.
- Sleep before midnight to synchronize melatonin, growth hormone, and thyroid function.
- Fast intermittently, but wisely—allowing the body periods of rest without triggering starvation signals.
- Move daily, but not obsessively—exercise reduces cortisol and increases endorphins.
- Breathe consciously, for oxygen is the first nutrient every cell receives.
Ritual, not rigidity, is the essence of hormonal health.
The Feminine and the Masculine Balance
Beyond biology, hormones embody archetypes—the yin and yang of human energy. Estrogen and progesterone cultivate receptivity, intuition, and nurturance; testosterone and growth hormone fuel assertion, strength, and ambition. Health arises not from one dominating the other but from their dialogue.
When society rewards constant output, masculine chemistry burns unchecked—cortisol, adrenaline, ambition. The result is burnout. When receptivity is neglected, the body forgets to rest, regenerate, and receive.
Healing, then, becomes a spiritual act as much as a physical one: restoring harmony between giving and receiving, between doing and being. In hormonal language, that means balancing action with restoration, light with dark, meal with fast, effort with grace.
Environmental Hormones — The Modern Disruptors
The modern world floods the bloodstream with endocrine disruptors: invisible chemicals that mimic or block hormones. They hide in plastics, personal care products, non-stick cookware, and pesticides. They impersonate estrogen, interfere with testosterone, and confuse thyroid receptors.
Reducing exposure begins with awareness—choosing glass over plastic, natural cosmetics over synthetic ones, organic produce over sprayed fields. The liver, again, becomes the hero; its detox pathways, fueled by cruciferous vegetables and hydration, metabolize these impostors before they rewrite the body’s instructions.
The endocrine system is ancient; pollution is new. Every choice that reduces chemical load is a vote for hormonal sovereignty.
Conclusion: Returning to the River
Hormones are not enemies to be controlled, but rivers to be respected. When they flow, the landscape of the body is fertile and clear. When they stagnate or flood, the terrain erodes. The task of modern health is not to dominate these rivers with medication or fear but to understand their tides—to know when to rest, when to eat, when to breathe, and when to listen.
The hormone highway is the body’s biography written in chemistry. It records every stress endured, every meal consumed, every joy remembered. To walk its path with awareness is to reclaim authorship over that story—to choose harmony over chaos, rhythm over noise, vitality over survival.
When the glands hum again in balance, the mind quiets, the skin glows, and life itself feels synchronized. That is not luck or youth—it is biology aligned with wisdom.
To balance hormones is to balance being. To eat with knowledge, rest with intention, and live with rhythm is to step back into the current of the body’s oldest truth: that every cell listens to the music we make when we live consciously.
Part 9: Immunity and Longevity — The Body’s Eternal Conversation

Longevity is not the absence of illness but the art of resilience. True immunity is not defense—it is dialogue.
Every living thing is born with a covenant: to survive, it must adapt. From the humblest cell to the human body, life’s central strategy has never been immortality, but renewal. Immunity is the expression of that ancient wisdom—a dynamic conversation between body and world, self and non-self, memory and mutation.
When this conversation flows smoothly, the body ages with grace; when it falters, the years accumulate as rust. Immunity, then, is the biology of longevity—not a fortress against disease, but a language of recognition, repair, and reinvention.
In a world of industrial diets, chronic stress, and artificial environments, this ancient language is being forgotten. The immune system, once trained by nature’s diversity, now fights phantoms—reacting to dust, food, and even itself. The result is paradoxical: societies that have conquered infections now face epidemics of autoimmunity, allergies, and chronic inflammation. The problem is notexposure—it is education.
To live long and well, we must reteach the body what it means to belong in its environment. That is the real meaning of immunity: not isolation, but intelligent connection.
Immunity as Intelligence
The immune system is not a single organ; it is a distributed intelligence. It lives in the bone marrow, where new soldiers are born; in the thymus, where they are trained; in the spleen and lymph nodes, where they strategize; and in the gut, where they meet the outside world.
Every breath, every bite, every cut is a test of discernment. The immune system must decide—instantly—what to tolerate and what to attack. Too lenient, and infection spreads; too vigilant, and self-destruction begins. This balance—between tolerance and aggression—is the biological foundation of peace.
But peace requires education. In infancy, microbes from soil, milk, and food teach the immune system what “safe” feels like. Children who grow up in overly sterile environments or consume processed diets often lack this microbial mentorship. Their immune systems remain naive, prone to panic. Hence the rise of asthma, eczema, and food sensitivities in the very societies that sterilized their kitchens.
Longevity begins with microbial wisdom. The body that knows how to distinguish friend from foe wastes less energy on false alarms and invests more in regeneration.
The Gut: Where Immunity Begins
Over 70% of the immune system resides in the gut-associated lymphoid tissue (GALT), the borderland where microbes, food, and immune cells negotiate peace. The gut’s lining, a single layer of cells, is both a wall and a window—porous enough to absorb nutrients, selective enough to block invaders.
Fermented foods—yogurt, kefir, ogi, kimchi, fermented cassava, and African locust-bean products—strengthen this frontier. They populate the gut with beneficial bacteria that produce short-chain fatty acids like butyrate, which nourish intestinal cells and regulate immune response. These molecules also travel beyond the gut, calming inflammation in distant tissues and even influencing brain chemistry.
When this microbial ecosystem is disrupted—by antibiotics, sugar, or ultraprocessed food—the gut wall weakens. Undigested particles slip through, confusing the immune system into launching attacks against harmless substances. This “leaky gut” is now recognized as a root cause of many autoimmune and inflammatory diseases.
Healing begins not in pharmacies but in kitchens that still honor fermentation, fiber, and freshness. Each spoonful of living food reintroduces ancient teachers to the modern gut.
The Inflammation Paradox
Inflammation is immunity’s first language—its way of responding to injury or infection. A bruise heals because inflammation cleanses and rebuilds. But when the signal never turns off, the body burns itself from within. Chronic inflammation is now recognized as the common denominator of aging, cancer, diabetes, heart disease, and dementia.
This persistent fire arises not from attack, but from confusion. Ultraprocessed foods, refined oils, and artificial additives keep the immune system on high alert, as if the body were under siege. Even psychological stress mimics infection, prompting the release of inflammatory cytokines.
Nature, however, offers antidotes. Polyphenols in fruits, omega-3 fats in fish, turmeric in curry, and antioxidants in leafy greens extinguish the flame gently, without suppressing immunity. A diet rich in plants and fermented foods recalibrates inflammation, reminding the immune system that not every stimulus requires war.
Longevity, therefore, is not about avoiding inflammation entirely—it is about mastering the art of its ending.
Africa’s Forgotten Blueprint for Longevity
Before nutrition was quantified, African diets practiced what science now preaches: microbial diversity, plant dominance, and cyclical fasting. Millet, sorghum, beans, yam, cassava, and fermented grains formed the foundation of health across the continent. Meals were seasonal, communal, and slow.
Today, researchers confirm that these traditional patterns support both immunity and lifespan. Fiber-rich, minimally processed foods feed beneficial bacteria that strengthen gut integrity and immune tolerance. Fermentation enhances vitamin bioavailability and introduces probiotic cultures that modern diets lack. Herbs like moringa, hibiscus, ginger, and bitter leaf provide antioxidant and antimicrobial compounds now being studied globally.
These foods do more than nourish—they communicate with genes, turning on pathways that reduce oxidative stress and promote cellular repair. In essence, they are epigenetic foods, teaching the body to express longevity.
What Africa once lived by intuition, modern science is rediscovering in the lab.
The Cellular Conversation of Aging
Every immune response leaves a trace—a memory. Over time, this memory accumulates, not only in immune cells but in the body’s entire cellular fabric. Aging, from this perspective, is not the passage of time but the residue of inflammation.
Each infection fought, each toxin encountered, each emotional wound adds to the ledger. When the body can no longer clear these residues, cells enter senescence—a state of suspended animation where they secrete inflammatory molecules but cease to divide. These senescent cells act like bad neighbors, poisoning their surroundings.
The key to longevity lies in teaching the immune system to recognize and remove these senescent cells efficiently. Diet again proves decisive. Nutrients like quercetin (found in onions and apples), resveratrol (in grapes and peanuts), and curcumin (in turmeric) activate genes responsible for cellular cleansing.
Longevity, then, is an immune achievement—the result of a body that remembers wisely and forgets in time.
The Role of Fermentation in Immune Longevity
Fermentation is one of humanity’s oldest biotechnologies, and perhaps its most brilliant. By allowing microbes to pre-digest food, fermentation transforms ordinary grains and vegetables into biochemical treasure. The process enhances vitamin content, produces organic acids, and introduces beneficial bacteria that colonize the gut.
In African food culture, fermentation was both necessity and medicine. Ogi (fermented maize porridge) supports infant immunity. Nunu (fermented milk) provides probiotics and enzymes. Dawadawa (fermented locust bean) enriches meals with amino acids and antioxidants. Even palm wine, in moderation, carries live yeast cultures that stimulate gut health.
Modern studies confirm that fermented foods reduce inflammatory markers, enhance antibody response, and improve resistance to viral infections. Regular consumption also correlates with lower rates of age-related diseases. The fermentation jar, it seems, is both kitchen and clinic.
In an era obsessed with sterility, fermentation reminds us that life thrives through collaboration, not isolation.
Micronutrients — The Immune Orchestra
No immune system can perform without its instruments: vitamins, minerals, and trace elements that tune its responses.
- Vitamin C strengthens white blood cells and accelerates tissue repair.
- Vitamin D acts as a master regulator, guiding immune memory and resilience.
- Zinc is the spark for hundreds of enzymatic reactions, including antiviral defense.
- Selenium protects cells from oxidative damage.
- Iron enables the transport of oxygen, the energy of immunity.
These nutrients often coexist in whole, natural foods—leafy greens, nuts, seeds, and legumes. Isolated supplements can help in deficiency, but only the synergy of real food delivers balance. The immune system does not crave doses; it craves diversity.
The Psychology of Resistance
The immune system listens not only to nutrients but to emotions. Chronic fear and anger suppress its function, while joy, connection, and purpose strengthen it. Laughter increases antibody production; loneliness diminishes it.
This psychoneuroimmunology—the science of how mind, nerve, and immunity intertwine—confirms what healers always knew: despair weakens the flesh, and hope revives it. Meditation, music, gratitude, and touch all signal safety to the nervous system, which in turn allows the immune system to shift from defense to regeneration.
Longevity is therefore not achieved by biology alone but by belonging—by the sense that one’s life still matters to others. In that sense, immunity is not only a personal asset; it is a social phenomenon.
Immunity as Ecology
The human body is not separate from its environment—it is an environment. The soil’s microbial health mirrors the gut’s. The air’s purity mirrors the lung’s. The loss of biodiversity outside predicts disease within.
Industrial agriculture, by sterilizing soil, has starved the human microbiome. Each lost microbe in the ground is a lost teacher for the immune system. Regenerative farming and clean water policies are therefore public health strategies as much as ecological ones.
To live long in a dying ecosystem is impossible. Longevity is an ecological contract, not a personal conquest.
The Blueprint for Immune Longevity
Immunity and longevity are not gifts of genetics but results of daily dialogue—between food and cell, mind and microbe, society and soil. To sustain that dialogue, one must return to the essentials:
- Eat food thatlives; fresh, colorful, and fermented.
- Sleep deeply, for the immune system rebuilds in darkness.
- Breathe slowly; oxygen is the oldest medicine.
- Connect often; community is immunity.
- Spend time in sunlight and soil—nature’s laboratories of life.
In these acts, simple yet profound, the immune system finds its rhythm again. And with it, aging becomes less of a decline and more of a deepening—a gradual mastery of the art of renewal.
The Immortal Conversation
Longevity is not about defying death; it is about amplifying life. The immune system does not exist to make us invincible, but to remind us that resilience is the essence of existence.
Each day the body rebuilds itself, cell by cell, molecule by molecule. The question is not whether we will age, but how we will participate in the dialogue between decay and regeneration. A well-fed microbiome, a calm mind, a diverse diet, and a meaningful life—all are forms of conversation with time.
To age with vitality is to keep that conversation alive, to listen as the body speaks softly through appetite, fatigue, and renewal. Immunity and longevity are not separate destinies—they are the same story told at different speeds.
When the immune system is wise, age becomes beauty, and time becomes teacher. The goal is not to live forever, but to live so well that the body never forgets how to heal.
Part 10: Healing the Mind Through the Gut — The Biology of Emotion
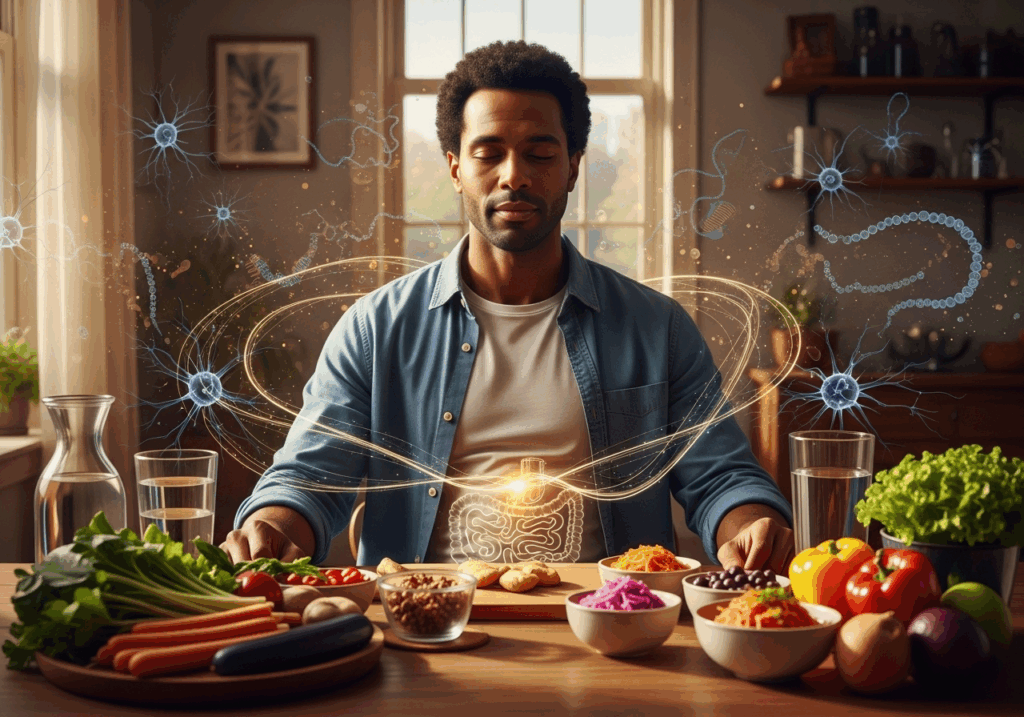
The gut does not whisper to the mind; it composes its music. Every thought begins with digestion, and every emotion leaves a trace in the intestines.
For generations, medicine treated the mind as an abstract cathedral—untouchable by the crude machinery of the body. Depression was a matter of neurotransmitters, anxiety a defect of psychology, and mood disorders the domain of psychiatry. Food, digestion, and microbes were considered too earthy, too mechanical, too trivial to shape consciousness.
That era is over.
The revolution now unfolding in neuroscience, immunology, and nutrition reveals a simple, almost subversive truth: the gut is not merely a digestive organ—it is an emotional organ. Its nerves, hormones, and microbial residents are inseparable from how we feel, think, and heal. Mental health, it turns out, begins in the microbiome.
The phrase “gut feeling” was never metaphorical—it was descriptive.
The Gut–Brain Superhighway
The human gut contains over 100 million neurons—more than the spinal cord. This vast network, known as the enteric nervous system, communicates constantly with the brain through the vagus nerve, the body’s longest information highway.
This two-way system is not symbolic. It is electrical, chemical, and hormonal. About 90% of serotonin—the neurotransmitter that regulates happiness, appetite, and sleep—is produced not in the brain, but in the gut. Dopamine, GABA, and norepinephrine—key molecules of motivation, calm, and focus—also originate in the microbiome’s chemical factories.
When the gut’s ecology is balanced, these messengers flow harmoniously. But when inflammation, stress, or processed food disrupt the microbial balance, these same signals become distorted. The result can be anxiety, brain fog, depression, irritability, or cognitive decline.
The gut and the brain are not two organs in conversation—they are one system speaking in two dialects.
Microbes as Mental Architects
Inside every human body lives a metropolis of trillions of bacteria, fungi, and archaea—the microbiome. These invisible citizens digest fiber, neutralize toxins, train immunity, and manufacture neurochemicals. They are the body’s first chemists and its most ancient psychologists.
Recent research has shown that people with diverse gut microbiota experience more emotional stability and resilience to stress. Those with depleted or imbalanced flora show higher rates of depression and anxiety. The mechanism is biochemical: beneficial bacteria produce short-chain fatty acids like butyrate, which reduce inflammation in the brain and protect the blood–brain barrier.
Conversely, a diet dominated by refined carbohydrates, seed oils, and synthetic additives feeds harmful microbes that release endotoxins. These toxins breach the intestinal wall, travel to the bloodstream, and trigger neuroinflammation—the silent saboteur behind many mental illnesses.
Thus, mental health is not only psychological; it is microbial.
The Food–Mood Equation
Every meal is a chemical event that either calms or agitates the mind. The Western diet, rich in sugar, trans fats, and ultraprocessed ingredients, has been consistently linked to higher rates of depression and anxiety. These foods inflame the gut, alter microbial diversity, and disrupt hormone signaling—particularly cortisol and insulin, both critical for mood regulation.
By contrast, diets emphasizing whole foods, fiber, healthy fats, and fermented products restore microbial harmony and emotional balance. The Mediterranean, Nordic, and many African indigenous diets share common threads: fresh produce, legumes, whole grains, and cultured foods that act as natural psychobiotics.
Fermented staples like ogi (soured maize), kenkey, nunu, and dawadawa deliver living bacteria that boost serotonin production. Leafy greens, yams, and beans supply magnesium and B vitamins that stabilize mood. Omega-3-rich fish oils reduce inflammation in neural tissue.
Every bite is a message to the nervous system: “You are safe,” or “You are under siege.”
Stress: The Great Disruptor
The modern world’s greatest toxin is not chemical—it is cortisol. Chronic stress alters gut motility, reduces microbial diversity, and damages the intestinal barrier. When stress persists, digestion slows, nutrient absorption declines, and inflammation rises.
This sets off a biochemical feedback loop: the inflamed gut sends distress signals to the brain, which amplifies anxiety and depression. The brain, in turn, releases more stress hormones, further disrupting digestion.
Healing this loop requires restoring the body’s natural rhythm of relaxation. Practices like deep breathing, meditation, prayer, yoga, and mindful eating activate the parasympathetic nervous system—the “rest-and-digest” mode that quiets inflammation and allows the gut to heal.
Stress management, therefore, is not a lifestyle luxury—it is a microbiological necessity.
The Nutritional Neurochemistry of Joy
To nourish the brain, one must first feed the gut. Each neurotransmitter depends on specific nutrients that the gut either produces or absorbs:
- Serotonin needs tryptophan, found in bananas, eggs, and legumes.
- Dopamine depends on tyrosine, found in seeds, nuts, and fish.
- GABA, the calming chemical, thrives on glutamine from whole grains and leafy vegetables.
- B vitamins, especially B6 and B12, act as coenzymes in neurotransmitter synthesis.
- Magnesium soothes the nervous system and prevents cortisol overload.
- Zinc sharpens focus and stabilizes mood.
When digestion is impaired or microbial diversity is low, these nutrients are poorly metabolized. This is why malnutrition of the gut leads to malnutrition of the mind, even in those who “eat well.” A balanced microbiome ensures that nutrients reach their destinations—and that the mind receives its fuel.
Fermentation and the Mind
Fermented foods are nature’s antidepressants. By converting simple ingredients into probiotic powerhouses, fermentation creates compounds that modulate the immune system, reduce inflammation, and produce serotonin precursors.
Studies on African fermented foods show that they harbor diverse bacterial strains—Lactobacillus, Bacillus subtilis, and Streptococcus thermophilus—which interact with gut cells to regulate brain signaling. These microbes produce gamma-aminobutyric acid (GABA), a neurotransmitter responsible for tranquility.
Traditional diets that incorporate fermented foods daily—such as dawadawa, ogi, fufu, and fermented vegetables—are rich in these psychobiotic agents. The result is not just digestive health, but emotional resilience.
Fermentation is a kind of alchemy: it transforms food into therapy, culture into consciousness.
Inflammation and the Depressed Brain
Emerging evidence reveals that depression is not merely a mental disorder—it is an inflammatory one. Elevated cytokines, leaky gut, and immune hyperactivity are common in patients with mood disorders. The gut–brain axis provides the missing link: inflammation in the intestines travels via the bloodstream to the brain, altering neurotransmitter pathways and dulling emotional regulation.
This is why anti-inflammatory diets often outperform synthetic antidepressants in long-term mental health outcomes. Foods rich in antioxidants—berries, turmeric, olive oil, green tea—protect the brain from oxidative stress. Omega-3 fats enhance neuron membrane fluidity, improving signal transmission. Polyphenols in cocoa and green vegetables lower cortisol and restore cognitive clarity.
To heal depression, one must quench the invisible fire in the gut.
Hormones, Microbes, and Mood
Hormones and microbes collaborate in an elegant choreography. Estrogen enhances the growth of beneficial gut bacteria, while gut bacteria regulate estrogen metabolism through the estrobolome—a microbial gene pool that determines how much estrogen reenters circulation. Imbalance in this system can lead to mood swings, fatigue, and anxiety.
Cortisol, too, depends on microbial health. A robust microbiome modulates stress hormone production, preventing overactivation of the hypothalamic-pituitary-adrenal (HPA) axis. The calmer the gut, the quieter the cortisol.
This symbiosis extends even to sleep: gut bacteria influence melatonin synthesis, ensuring the body maintains circadian balance. When this cycle falters, insomnia and emotional exhaustion follow.
The endocrine and microbial systems are, in truth, one continuous dialogue—a biological chorus that sings the mind into harmony or despair.
Micronutrients and the Mental Immune System
Micronutrients are the invisible bridges between gut health and mental health. Deficiency in zinc, vitamin D, magnesium, or B12 can trigger fatigue, anxiety, and cognitive decline. These nutrients shape not only the nervous system but the microbial community itself.
For instance, zinc deficiency favors the growth of pathogenic bacteria; magnesium deficiency heightens stress response; low vitamin D impairs microbial diversity. Correcting these imbalances is not a supplement strategy—it is a restoration of cellular democracy.
A well-nourished gut microbiome is the immune system of the mind, defending against despair and restoring equilibrium after trauma.
The Emotional Microbiome
Every emotion leaves a chemical trace in the gut. Anger tightens the intestines; grief slows digestion; joy increases peristalsis. The microbes, in turn, respond—releasing molecules that either perpetuate or soothe those emotions. The result is a feedback loop between psychology and physiology, spirit and cell.
This is why traditional healing practices often link food, mood, and ritual. Communal meals, prayer before eating, and gratitude rituals all calm the nervous system and prepare digestion. Modern science now recognizes what ancient cultures practiced intuitively: emotional state determines digestive efficiency.
To heal the gut is to process emotion. To eat consciously is to meditate with the mouth.
The Path to Mental Restoration
Healing the mind through the gut requires an integrated approach—neither purely nutritional nor purely psychological. It is a philosophy of nourishment that honors biology as much as belief.
- Eat foods that live—fermented, colorful, unprocessed.
- Fast occasionally to reset microbial cycles.
- Hydrate deeply; water is the conductor of electrical balance.
- Sleep before midnight; microbiota regenerate with circadian rhythm.
- Move often, for movement stirs both lymph and emotion.
- Laugh, connect, forgive—each act produces neurotransmitters.
In these simple acts, the gut learns peace, and the mind rediscovers clarity.
Conclusion: The Mind Below the Heart
The frontier of mental health does not lie in laboratories but in the abdomen. Beneath the ribs and above the pelvis, the gut hums with thoughts unspoken—bacterial, chemical, and emotional. When it is nourished, the mind feels light; when it is wounded, the world darkens.
The gut is the mind’s memory of the body. It stores every trauma, every feast, every fast, every forgotten emotion. To heal it is to rewrite the body’s autobiography in new language—a language of fiber, fermentation, and forgiveness.
The most radical act of self-care is not therapy, medication, or meditation alone—it is the daily meal eaten with awareness, gratitude, and balance. The next revolution in psychiatry will not begin in the brain; it will begin in the kitchen.
The gut does not simply sustain life—it interprets it.
And when we feed it wisely, it teaches the mind how to feel whole again.
Part 11: Food Justice and the Politics of Health — Who Owns the Right to Eat?

Health is not just a biological condition; it is a political outcome. Food is not merely sustenance—it is power, policy, and profit.
The story of food has never been neutral. Every grain of rice, every loaf of bread, every drop of oil that reaches a table passes through invisible structures of control—policies, corporations, and systems that decide who eats well, who eats little, and who eats poison in the name of convenience. Across the world, and particularly in Africa, food has become the most silent yet potent form of inequality.
The supermarket shelf is not a marketplace—it is a mirror of power. Behind each brand lies a chain of ownership that stretches from multinational boardrooms to exploited farmlands. Behind each label that reads “organic” or “fortified” lies a political choice about who deserves nourishment and who does not.
To speak of food justice is to challenge this imbalance. It is to demand that nutrition, like oxygen, be recognized as a human right, not a commercial privilege.
The Politics Beneath the Plate
Food is a social contract between citizens and the state. Governments that fail to feed their people fail in their most basic obligation. Yet, across much of the developing world, policy favors profit over public health. Subsidies pour into industrial agriculture and chemical fertilizers while traditional crops—millet, sorghum, cassava, yam—receive little support despite their resilience and nutrition density.
In African cities, imported wheat and rice displace local grains; fast-food chains multiply while smallholder farmers vanish. This is not globalization—it is dependency repackaged as modernity.
Food systems reflect politics as much as economics. The nutritional deficit of nations mirrors their governance deficit: opaque policies, captured ministries, and development models designed for export markets rather than local sustenance.
The tragedy is structural. Multinationals dominate seed distribution, fertilizer access, and commodity pricing. When farmers buy genetically modified seeds, they enter cycles of dependence. When governments import food, they import vulnerability. The sovereignty of the stomach becomes the last frontier of colonization.
Heritage Diets and the Economics of Displacement
Before industrial agriculture, Africa, Asia, and Latin America sustained themselves on heritage diets—plant-rich, seasonal, and adaptive to local ecologies. These diets balanced macronutrients naturally, supported biodiversity, and required no chemical intervention. They represented not only nutrition but cultural identity and ecological wisdom.
Today, the global food economy erases these heritages in favor of uniformity. The “modern” diet—high in refined flour, sugar, and oils—spreads like a silent epidemic, carrying obesity, diabetes, and heart disease in its wake.
What scientists now call the nutrition transition is, in truth, a political transition: from autonomy to dependency, from communal farming to corporate monoculture. As heritage diets vanish, so too does cultural self-determination. The recipes of grandmothers are replaced by slogans of corporations; flavor yields to profit.
Yet, within these lost traditions lies the medicine modernity desperately seeks. African fermented foods, Mediterranean plant-based cuisines, and Asian heritage diets all share one principle: equilibrium between nature, body, and society. The erosion of that balance is not inevitable—it is engineered.
The Corporate Capture of Hunger
To understand global nutrition inequity, one must follow the money. The world’s largest agribusinesses—few in number, vast in reach—control nearly every step of the food chain: seeds, inputs, distribution, and even public health messaging.
These corporations present themselves as allies in the fight against malnutrition, yet their products often perpetuate it. Fortified processed foods marketed to poor populations replace fresh produce. Artificially sweetened beverages replace clean water. Subsidized instant noodles flood markets where traditional grains once thrived.
Food deserts—urban zones where healthy food is scarce—are not accidents. They are policy outcomes. When profit dictates geography, the poor pay with their bodies. In the same neighborhood, one finds cheap calories but expensive nutrition—a system where obesity and hunger coexist at the same table.
Health becomes a matter of purchasing power, not policy protection.
Inflammation as a Social Condition
The body’s inflammation is the planet’s inflammation. The same systems that poison soil and water also poison blood and organs. Industrial food systems that depend on pesticides, synthetic fertilizers, and ultraprocessing not only erode the environment but ignite chronic disease.
Inflammation is the body’s protest—a physiological echo of political neglect. It is how the body says, “I am being poisoned.”
From the high-sugar diets of urban poor communities to the air-polluted environments of industrial zones, public health crises cannot be separated from economic models. The rise of diabetes and heart disease in Africa and Asia is not merely a lifestyle issue—it is the biochemistry of inequality.
As Harvard Health and Nutrition.org emphasize, anti-inflammatory diets—rich in fruits, legumes, whole grains, and healthy oils—reduce disease risk dramatically. Yet, these very foods are the least accessible to those who need them most. The politics of food ensures that what heals is priced high, and what harms is cheap.
Food justice, then, begins with making healing affordable.
Knowledge as Liberation
Every revolution begins with knowledge. In the realm of food, ignorance is the most profitable commodity. Advertising convinces the poor that foreign snacks equal progress; policy convinces farmers that monocrops equal modernity. The result is a disempowered populace that no longer trusts its indigenous wisdom.
Reviving food justice requires re-educating both farmers and consumers. It means teaching that traditional grains are superfoods, not relics; that fermented foods preserve life, not poverty; that biodiversity is wealth, not backwardness.
As Prof. Ruth Oniang’o and other nutrition scholars have shown, Africa’s contribution to global sustainable diets lies not in imitation but in rediscovery. The continent’s culinary biodiversity—leafy greens, legumes, tubers, and natural fermentations—offers models for sustainable, climate-resilient nourishment.
To restore justice, knowledge must move from laboratories to communities, from ministries to markets, from slogans to soil.
The Gender Dimension
Food injustice is gendered. Across Africa and much of the developing world, women are both the primary food producers and the least nourished. They cultivate, harvest, cook, and sell—but seldom own land or control pricing. Policies that ignore women’s access to credit, markets, and technology deepen both poverty and malnutrition.
Yet women’s empowerment is the single most reliable catalyst for nutritional transformation. When women farmers control income, child malnutrition drops. When women lead food cooperatives, biodiversity rises. When women educate, diets diversify.
Food justice cannot exist without gender justice. To feed a nation, one must first feed its women with power.
Food Policy as Moral Architecture
Every food system is an ethical architecture—a set of moral decisions encoded in policy. The choice to subsidize refined sugar but not vegetables is a moral decision. The decision to allow pesticide residues but tax small farmers is a moral decision.
True food justice demands political courage:
- Redistributive subsidies, shifting support from export crops to local staples.
- Regenerative agriculture, investing in soil as living capital.
- Transparent labeling, so citizens know what they consume.
- Corporate accountability, ensuring that public health outweighs profit.
Governments must understand that food policy is health policy. A nation’s hospitals are only as effective as its farms. A nation’s GDP is only as sustainable as its nutrition base.
The Colonial Legacy of the Stomach
Colonialism was not only a political conquest; it was a dietary one. Colonizers imposed foreign crops, foreign tastes, and foreign dependencies. Wheat displaced millet; sugar replaced honey; imported oils overtook palm and sesame. Even after independence, food aid and trade policies preserved these hierarchies.
The colonized palate persists—a psychological inheritance of inferiority that values imported brands over native nourishment. Food justice is, therefore, a form of decolonization—a reclaiming of taste, seed, and sovereignty.
To eat locally and consciously is an act of political defiance.
The Future of Food Freedom
Food justice must evolve from protest to policy, from activism to architecture. The path forward lies in:
- Agroecology, which harmonizes production with ecosystem balance.
- Community-owned food systems, where farmers share profits and knowledge.
- Cultural nutrition education, which revives traditional diets in urban schools.
- Digital transparency, allowing citizens to track food origins and corporate behavior.
Above all, food justice requires empathy—the recognition that hunger anywhere diminishes humanity everywhere.
Conclusion: The Right to Dignified Eating
To heal the world, one must begin at the table. Food is not merely a calorie count—it is a covenant between body and planet, between citizen and state. The politics of health begins not in hospitals but in kitchens, farms, and markets.
When people reclaim the right to real food—clean, local, fair—they reclaim the right to live with dignity. The revolution will not be televised; it will be cooked, shared, and eaten.
Part 12: The Kitchen as Clinic — Where Healing Begins Before Illness

The most powerful form of medicine is not swallowed but served. The kitchen, not the clinic, is the first hospital; the cook, not the chemist, is the first healer.
There was a time when the act of cooking was sacred—a ritual of preservation, protection, and love. Food was not merely sustenance but medicine, an everyday covenant between body and nature. The healer’s wisdom was transmitted not through prescriptions but through recipes. A mother’s broth treated fever; a grandmother’s tea calmed the gut; spices served as syringes of immunity.
Then came industrialization, and the kitchen lost its authority. Healing moved from the home to the hospital, and food was demoted from medicine to commodity. The modern diet became efficient but lifeless, convenient but corrosive. We began to outsource nourishment to corporations and wellness to pharmacology.
Yet, as global disease burdens rise—from diabetes and heart disease to anxiety and autoimmune disorders—the world is returning, quietly but urgently, to its oldest clinic: the kitchen.
The Biochemistry of the Stove
The kitchen is not a place of routine—it is a biochemical laboratory. Every ingredient, every temperature, every combination creates a chain reaction in the body. When we chop garlic, we release allicin, a compound that lowers cholesterol and blood pressure. When we simmer tomatoes in olive oil, we unlock lycopene, a cancer-fighting antioxidant. When we ferment cabbage into sauerkraut, we cultivate lactobacilli, guardians of the gut.
Cooking is chemistry disguised as art. It determines how nutrients are absorbed, how hormones respond, and how inflammation behaves. Boiling, roasting, and fermenting are not simply culinary techniques—they are modes of medicine.
Scientific studies now confirm what ancestral wisdom always knew: the way food is prepared changes its medicinal power. Raw kale is fibrous and indigestible to some, but when steamed lightly, its antioxidants become bioavailable. Turmeric releases its curcumin only when heated with fat and pepper. Bone broth becomes collagen therapy when simmered for 12 hours.
In this alchemy of flame and flavor, the kitchen restores its ancient role as pharmacy.
Food as Code: The Molecular Language of Healing
Inside every meal lies a set of instructions—a molecular script that tells the body how to function, repair, and defend itself. Proteins, fats, and carbohydrates are not just calories; they are messages. The body reads these messages through receptors, enzymes, and hormones.
For instance, when you eat whole grains, your gut releases short-chain fatty acids that regulate gene expression linked to inflammation and metabolism. When you consume polyphenol-rich foods—berries, green tea, cocoa—your body activates antioxidant pathways that protect DNA.
Every forkful is an act of gene editing. You are not simply eating; you are programming your biology.
The kitchen, therefore, is where epigenetics becomes everyday practice. It is where the family DNA is either strengthened or sabotaged. Disease prevention does not begin in diagnostics—it begins in dinner.
Micronutrients: The Invisible Healers
Modern nutrition often obsesses over macronutrients—carbs, fats, proteins—but it is the micronutrients that perform the miracles. These trace elements and vitamins are the body’s unsung orchestra: silent, subtle, indispensable.
Magnesium regulates over 300 enzymatic reactions, calming nerves and balancing glucose. Zinc accelerates wound healing and immune repair. Selenium acts as a shield against oxidative stress. Iron ferries oxygen; iodine sculpts hormones.
Deficiency in any one micronutrient can derail dozens of bodily systems. The symptoms—fatigue, depression, skin issues, insomnia—are often misdiagnosed as unrelated illnesses. But the cure may not lie in medication; it may lie in mineral balance.
Real food delivers these micronutrients in perfect ratios. A handful of nuts supplies magnesium and selenium. Leafy greens deliver folate and potassium. Eggs and liver provide choline and iron. Fermented foods enhance vitamin B synthesis naturally.
When you cook whole foods, you’re not feeding hunger—you’re conducting molecular therapy.
Fermentation: The Ancient Prescription
Long before probiotics had a name, fermentation was humanity’s insurance policy against disease. The process was as spiritual as it was scientific—a collaboration between human ingenuity and microbial intelligence.
Fermented foods are alive. They host beneficial bacteria that strengthen the immune system, balance hormones, and reduce inflammation. Modern research confirms that these microbes produce neurotransmitters like serotonin and dopamine—chemicals once thought exclusive to the brain.
In Africa, the tradition of fermentation remains vibrant. Ogi, nunu, dawadawa, and kenkey are not just staples; they are symbiotic systems of health. Their microbes improve nutrient absorption and detoxify harmful compounds. They preserve food without refrigeration and enrich diets without additives.
Each bowl of fermented grain or dairy is a living culture of healing. The kitchen becomes a probiotic lab, the cook a microbiologist without a microscope.
Hormones and the Healing Table
Hormones are the body’s internal broadcasters—chemical messages that dictate everything from appetite to emotion. What we eat determines how loudly they speak and what they say.
Balanced meals—those with fiber, protein, and healthy fats—stabilize insulin and cortisol, the twin gatekeepers of metabolic and emotional stability. Spikes in blood sugar lead to hormonal chaos: fatigue, irritability, and weight gain. Chronically high cortisol, fueled by stress and refined sugar, suppresses immunity and accelerates aging.
Certain foods naturally restore balance. Cruciferous vegetables like broccoli and cabbage aid estrogen metabolism. Omega-3 fats in fish regulate leptin and ghrelin, the hormones of hunger and satiety. Zinc and B6 support testosterone and progesterone synthesis.
Each meal is a hormonal symphony—or a hormonal storm. The kitchen decides which.
Cellular Youth and Culinary Longevity
Aging, at its essence, is the accumulation of cellular damage. But what if cooking could slow that clock?
Science reveals that certain dietary compounds activate longevity genes—sirtuins and AMPK—that govern repair and renewal. Foods rich in resveratrol (grapes, peanuts), curcumin (turmeric), and quercetin (onions, apples) mimic the effects of calorie restriction, promoting cellular regeneration.
Fermented foods extend this effect by reducing oxidative stress and maintaining mitochondrial health. Whole grains, legumes, and antioxidants feed the gut microbes that, in turn, produce anti-aging compounds.
The kitchen, then, is a time machine. In each pot of soup simmered slowly, in each salad dressed with olive oil, the molecular machinery of youth hums back to life.
The Gut as Diagnostic Tool
In a world obsessed with medical tests, the gut remains the body’s most accessible diagnostic device. Its signals—bloating, cravings, fatigue, or mood swings—reveal internal imbalances long before lab results do.
When you cook consciously, you become your own clinician. You learn to read your body’s feedback not as nuisance but as guidance. A bloated stomach after bread might indicate gluten sensitivity; craving salt may signal mineral deficiency; sugar cravings can reflect dysbiosis or stress.
This self-awareness transforms the kitchen into a place of observation and adjustment—a feedback loop of healing.
The Ritual of Preparation
Cooking is more than science—it is meditation. The sensory rhythm of washing vegetables, grinding spices, and stirring soups reawakens the nervous system’s calm pathways.
When cooking is performed with mindfulness, it lowers stress hormones, slows breathing, and enhances digestion. The act of preparing food becomes an act of presence—a dialogue between hand, heart, and hunger.
The best healers in history understood this: intention flavors food. Gratitude before meals aligns the body’s biochemistry toward peace. Anger while cooking, stress while eating—these are toxins that no detox can cure.
To cook consciously is to practice preventive medicine.
Medicine Reimagined
The clinical world often treats food as an adjunct to treatment—secondary to drugs and surgery. But the evidence is overwhelming: 70% of chronic diseases are preventable through diet and lifestyle alone. Type 2 diabetes, hypertension, and even early-stage autoimmune disorders can be reversed with sustained nutritional therapy.
The kitchen can do what prescriptions cannot—it can create habit. Habits heal because they make health automatic. The consistency of daily choices, not the intensity of medical interventions, determines long-term wellness.
If every home cooked with awareness, hospitals would lose half their patients.
From Recipe to Revolution
The idea of the “kitchen as clinic” is not nostalgia—it is a global movement. Nutritionists, physicians, and chefs are converging around culinary medicine, an emerging field that trains healthcare workers to prescribe food with the same precision as pharmaceuticals.
Hospitals in the United States, Europe, and Asia now host teaching kitchens where patients learn to cook their way out of chronic disease. In Africa, community programs are reintroducing traditional foods as tools for both economic empowerment and public health.
The revolution will not only be televised—it will be sautéed, fermented, and served.
The Moral of the Meal
Food is the most democratic medicine: available daily, shared communally, and capable of transformation. But its power depends on participation. The kitchen is not a passive space—it is a battleground between healing and harm, between industry and integrity.
Each meal asks a moral question: Will this nourish life or erode it? Will it sustain the planet or deplete it? Will it connect me to others or isolate me in convenience?
To choose food consciously is to vote for a future where health is a shared inheritance, not a private luxury.
Conclusion: Returning the Clinic Home
The clinic of tomorrow does not need to be invented—it already exists, tiled in smoke and spice, humming with the aroma of restoration. The stove is its altar; the cutting board, its laboratory; the dining table, its therapy room.
When we reclaim the kitchen, we reclaim autonomy over our health. We cease to be patients and become participants in our healing.
The prescription is simple:
- Cook more, buy less.
- Eat what is alive.
- Use food to converse with your biology, not silence it.
The future of medicine will not come in a capsule—it will come in a bowl.
Bibliographies
Berger, M. M. (2024). The science of micronutrients in clinical practice. Clinical Nutrition, 43(2), 123–134.
Calubag, M. F., Lee, S., & Park, H. (2024). Dietary macronutrients and cellular senescence. Cell Metabolism. Retrieved October 22, 2025, from https://www.sciencedirect.com/science/article/pii/S1550413124003279
Cantelli, F. (2025, February 11). Past and future of the Mediterranean diet: How models can adapt to local needs. OnFoods Magazine. Retrieved October 22, 2025, from https://onfoods.it
Cart, C. (2025). Nutrition and impacts on hormone signaling. Institute for Functional Medicine. Retrieved October 22, 2025, from https://www.ifm.org/articles/nutrition-impacts-hormone-signaling
Espinosa-Salas, S. (2023). Nutrition: Micronutrient intake, imbalances, and interventions. NBK Bookshelf. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK597352
Food & Nutrition Bulletin. (2025). Africa’s contribution to global sustainable and healthy diets. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/articles/PMC12083016
Frontiers in Medicine. (2022). Ultra-processed foods as a possible culprit for the rising prevalence of IBD. Frontiers in Medicine. Retrieved October 22, 2025, from https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1058373/full
Frontini, E. (2023). Ultra-processed foods, inflammation, and the battle for heart health. BMJ, 384, e077310.
Godos, J., Martinez-Gonzalez, M. A., & Grosso, G. (2024). Underrated aspects of a true Mediterranean diet. Journal of Translational Medicine, 22, 50. https://doi.org/10.1186/s12967-024-05000
Harvard Health Publishing. (2023). Foods that fight inflammation. Harvard Health Publishing. Retrieved October 22, 2025, from https://www.health.harvard.edu/staying-healthy/foods-that-fight-inflammation
HealthLine. (2025). 10 natural ways to balance your hormones. HealthLine. Retrieved October 22, 2025, from https://www.healthline.com/nutrition/balance-hormones
Jeyaram, K., Li, Y., & Chen, T. (2025). Fermented foods affect the seasonal stability of gut bacteria. Nature Communications. Retrieved October 22, 2025, from https://www.nature.com/articles/s41467-025-56014-6
Le Blanc, K. E., Santos, J., & Rivera, P. (2024). Beyond the Mediterranean diet—Exploring Latin American, Asian, and African heritage diets. Advances in Nutrition, 15(4), 711–722.
Lee, G., Han, S., & Zhao, T. (2025). Post-ingestive systemic nutrient sensing for whole-body regulation. Trends in Endocrinology & Metabolism. Retrieved October 22, 2025, from https://www.sciencedirect.com/science/article/pii/S1016847825000950
Louw, N. L., Venter, J., & Ofoegbu, C. (2023). Microbiome assembly in fermented foods. Annual Review of Microbiology. Retrieved October 22, 2025, from https://www.annualreviews.org/content/journals/10.1146/annurev-micro-032521-041956
Malongane, F., Mokhele, T., & Baloyi, M. A. (2024). Exploring the microbiome present in fermented indigenous African foods and beverages. Food Science & Nutrition. Retrieved October 22, 2025, from https://www.sciencedirect.com/science/article/pii/S2666154324001388
Mazza, E., Frontini, E., & Rossi, M. (2024). Obesity, dietary patterns, and hormonal balance modulation. Nutrients. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/articles/PMC11174431
Morris, A. L. (2023). Biochemistry, nutrients. StatPearls. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK554545
Nature Communications. (2025). Fermented foods affect the seasonal stability of gut bacteria. Nature Communications. Retrieved October 22, 2025, from https://www.nature.com/articles/s41467-025-56014-6
Nutrients. (2023). The detrimental impact of ultra-processed foods on the human gut microbiome and gut barrier. Nutrients, 17(5), 859. https://doi.org/10.3390/nu17050859
Nurkolis, F., Widyastuti, N., & Rahman, A. (2025). New insight on dietary strategies to increase insulin sensitivity and reduce diabetes prevalence. Discover Food, 5, 136.
Nutrition.org. (2021). The link between diet, inflammation, and disease. American Society for Nutrition. Retrieved October 22, 2025, from https://nutrition.org/the-link-between-diet-inflammation-and-disease
Obafemi, Y. D., Adebiyi, A. O., & Ogundele, O. M. (2022). African fermented foods: Overview, emerging benefits, and future potential. npj Science of Food, 6, 45.
Oniang’o, R. (2025). Africa’s contribution to global sustainable and healthy diets. Food & Nutrition Bulletin. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/articles/PMC12083016
Valentino, V., Brambilla, D., & Rossi, G. (2024). Fermented foods, health and the gut microbiome. Food & Nutrition Bulletin. Retrieved October 22, 2025, from https://www.ncbi.nlm.nih.gov/articles/PMC9003261
Yale Medicine. (2024). Are ultra-processed foods bad for your health? Yale Medicine. Retrieved October 22, 2025, from https://www.yalemedicine.org/news/ultraprocessed-foods-bad-for-you